Hamstring Origin Tendonitis (Tendinopathy)
Updated:
(Also known as Hamstring Origin Tendonitis, Hamstring Origin Tendinopathy, Proximal Hamstring Tendinopathy, Hamstring Tendonitis, Hamstring Tendinopathy, Hamstring Tendinitis)
N.B. Although research suggests that ‘hamstring tendinopathy’ is the more appropriate term to describe overuse injuries to the hamstring tendon (due to the absence of an inflammatory response), we will use the term ‘hamstring tendonitis’ in this document as it is more commonly known.
What is hamstring origin tendonitis?
Hamstring origin tendonitis (tendinopathy) is a condition characterised by tissue damage, swelling and degeneration of the hamstring tendon (at its attachment to the pelvis) causing pain in the buttock.
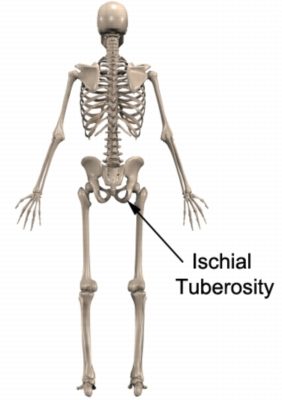
The hamstring muscles originate from the pelvis at the lower aspect of the buttock (ischial tuberosity i.e. sit bones – figure 1) and insert into the top of the lower leg bones (tibia and fibula). The hamstring muscles attach to the ischial tuberosity via the proximal (upper) hamstring tendon (figure 2).
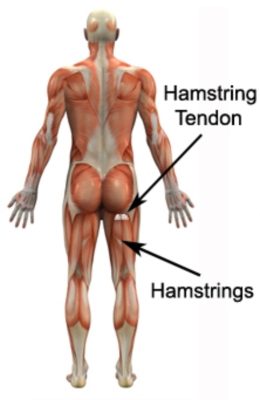
The hamstring muscles are responsible for bending the knee and straightening the hip during activity and are particularly active during running, jumping, squatting, lunging and kicking. During contraction and stretch of the hamstrings, tensile and compression forces are placed upon the proximal hamstring tendon. When these forces are excessive due to too much repetition, prolonged or high force, damage to the hamstring tendon occurs.
Hamstring origin tendonitis (tendinopathy) is a condition typically involving some or all of the following tendon changes:
- microscopic damage
- degeneration
- collagen fibre disorganisation (the protein giving tensile strength to the hamstring tendon)
- tendon swelling
- thickening of the tendon
- growth of new blood vessels (neovascularization) and nerves
Collectively, these changes reduce the tendon’s capacity to tolerate tensile and compression forces and increase the pain sensitivity of the tendon.
3 Phases of Hamstring Origin Tendonitis (Tendinopathy)
Following an inability of the hamstring tendon to appropriately adapt to an increase in stress on the tendon, hamstring origin tendonitis (tendinopathy) typically progresses through 3 phases:
- Reactive Phase – Comprising a short term adaptation to stress. This thickens the tendon, increasing its stiffness and reduces stress. Tendon changes during the acute reactive phase are typically reversible (with appropriate management). Generally the tendon structure remains intact.
- Dysrepair Phase – If the reactive tendon continues to be exposed to excessive load, further changes will take place within the tendon. These changes include a breakdown in the structure of the tendon. New blood vessels and nerves also begin to grow resulting in an increase in pain and sensitivity of the tendon. Appropriate treatment and load management during this phase is essential to prevent further progression to the degenerative phase.
- Degenerative Phase – This involves changes in response to long term overload of the tendon. These changes include further breakdown in the tendon structure, disorganisation of collagen fibres and areas of cell death. Additional growth of new blood vessels and nerves occurs. During this phase, the tendon may appear thickened or nodular and be at a higher risk or rupture.
Causes of hamstring origin tendonitis
Hamstring origin tendonitis (tendinopathy) most commonly occurs due to a sudden increase in repetitive or prolonged activities placing strain and in particular, compressive forces on the hamstring tendon. This typically occurs during activities that contract the hamstrings, particularly when they are in a position of stretch.
Hamstring origin tendonitis is common in athletes involved in distance running (particularly up hills), hurdles, football, sprinting, cycling, jumping activities and hockey. Occasionally, hamstring origin tendonitis may occur suddenly due to a high force going through the hamstring tendon beyond what it can withstand. This most commonly occurs during rapid acceleration whilst running or when a footballer performs a long kick. In the non-athletic population, hamstring origin tendonitis may occur in association with excessive sitting periods (particularly with the leg outstretched e.g. driving) or excessive hamstring stretching (e.g. Yoga).
Signs and symptoms of hamstring origin tendonitis
Patients with hamstring origin tendonitis typically experience fairly localised pain or discomfort in the lower buttock. Symptoms are usually located just below the sit bones (ischial tuberosity – figure 1), corresponding with the hamstring tendon location (figure 2). In less severe cases of hamstring origin tendonitis, patients may only experience an ache, stiffness or tightness in the lower buttock that increases with rest following activities requiring strong, repetitive or prolonged contraction or stretch of the hamstring muscle. These activities may include:
- running
- jumping
- kicking
- squatting
- lunging
- prolonged sitting (especially on hard surfaces)
- hamstring stretching
- excessive walking (particularly up hills or stairs)
- leaning forwards activities (e.g. housework, gardening etc.)
The pain associated with hamstring origin tendonitis often warms up with activity in the initial phase of the condition. As the condition progresses, patients with hamstring origin tendonitis may experience symptoms that increase during activity and affect performance. Patients with hamstring origin tendonitis often experience pain on firmly touching the hamstring tendon (figure 2). Occasionally, a feeling of lower limb weakness may also be present particularly when attempting to accelerate whilst running.
Diagnosis of hamstring origin tendonitis
A thorough subjective and objective examination from a physiotherapist is usually sufficient to diagnose hamstring origin tendonitis. Occasionally, further investigations such as an Ultrasound, X-ray or MRI scan may be required to assist with diagnosis and assess the severity of the hamstring origin tendonitis.
Prognosis of hamstring origin tendonitis
Most patients with hamstring origin tendonitis (tendinopathy) heal well with appropriate physiotherapy and return to normal function in a number of weeks (particularly those in the acute reactive phase). Occasionally, rehabilitation can take significantly longer and may take many months in those who have progressed to the dysrepair and degenerative phases. Early physiotherapy treatment is vital to hasten recovery in all patients with hamstring origin tendonitis.
Treatment for hamstring origin tendonitis

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Contributing factors to the development of hamstring origin tendonitis
There are several factors which can predispose patients to developing hamstring origin tendonitis. These need to be assessed and corrected with direction from a physiotherapist. Some of these factors include:
- joint stiffness (particularly the hip)
- muscle tightness (particularly the hamstrings, hip flexors and quadriceps)
- inappropriate or excessive training, stretching or activity
- inadequate warm up
- muscle weakness (especially the hamstrings, gluteals and quadriceps)
- poor pelvic or core stability
- inadequate rehabilitation following a previous hamstring injury
- leg length discrepancies
- female gender
- increasing age
- obesity
- history of another lower limb injury
- sciatic nerve irritation
- poor sporting technique
- fatigue
Physiotherapy for hamstring origin tendonitis
Physiotherapy treatment for hamstring origin tendonitis is vital to hasten the healing process, ensure an optimal outcome and reduce the likelihood of recurrence. Treatment may comprise:
- education
- activity modification advice
- anti-inflammatory advice
- exercises to improve strength, core stability and flexibility
- soft tissue massage
- dry needling
- electrotherapy (primarily for pain relief)
- joint mobilisation
- ice or heat treatment
- clinical Pilates
- a gradual return to running program
- a gradual return to activity program
Other intervention for hamstring origin tendonitis
Despite appropriate physiotherapy management, some patients with hamstring origin tendonitis (tendinopathy) do not improve adequately. When this occurs the treating physiotherapist or doctor will advise on the best course of management. This may include further investigations such as X-rays, ultrasound, MRI or CT scan, pharmaceutical intervention, corticosteroid injection, platelet rich plasma injections, extracorporeal shockwave therapy or referral to appropriate medical authorities who will advise on any interventions that may be appropriate to improve the hamstring origin tendonitis.
Exercises for hamstring origin tendonitis
The following exercises are commonly prescribed to patients with hamstring origin tendonitis. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed as directed and only provided they do not cause or increase symptoms.
Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate and advanced exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place gradually and provided there is no increase in symptoms.
Initial Exercise
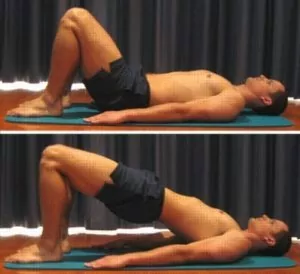
Bridge Holds
Begin this exercise lying on your back in the position demonstrated (figure 3). Slowly lift your bottom pushing through your feet, until your knees, hips and shoulders are in a straight line. Hold this position initially for 10 seconds then slowly lower your bottom back down. Gradually build up to 45 second holds over a number of days, allowing an equal rest period between repetitions. Perform 3 – 5 repetitions provided the exercise is pain free. Repeat 2 – 3 times per day.
Intermediate Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Advanced Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Other Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Rehabilitation Protocol for hamstring origin tendonitis
The following is a general rehabilitation protocol for patients with hamstring origing tendonitis (tendinopathy). This needs to be tailored to each individual and should be discussed with your treating physiotherapist prior to commencing. Progression through this program can vary from numerous days to many months depending on injury severity and quality of treatment:
- See your physiotherapist as soon as possible to confirm diagnosis, establish the likely prognosis, identify the contributing factors to injury and begin appropriate treatment.
- Follow the R.I.C.E. Regime for the first 48 – 72 hours following injury onset and if signs of acute injury are present (i.e. night-time pain, morning ache/stiffness or pain at rest). This should primarily comprise:
- Rest from any activity that increases pain either during activity or after that activity with rest (such as the next night or morning). If walking is painful or causing a limp, the use of crutches are usually required.
- Ice the sore area for 20 minutes and repeat every 2 hours (e.g. an ice pack wrapped in a damp tea towel)
- Anti-inflammatory medication (specifically ibuprofen) may be beneficial (discuss this with your doctor and/or pharmacist)
- The use of crutches, is usually indicated if walking is painful or causing a limp.
- Settle symptoms – continue to rest from any activity that increases pain during the activity or after that activity with rest (e.g. the following night or morning). Activities which place large amounts of stress through the hamstrings should also be minimised, particularly:
- running
- jumping
- kicking
- squatting
- lunging
- prolonged sitting (especially on hard surfaces)
- hamstring stretching
- excessive walking (particularly up hills or stairs)
- leaning forwards activities (e.g. housework, gardening etc.)
- If using crutches, walk normally, but take enough weight off the injured leg so walking is pain free and limp free. Sometimes smaller steps may be required for a period of time. Gradually increase weight through the injured side as tolerated provided there is no increase in pain or limp until eventually you can walk with only one crutch (using the crutch on the opposite side of the body to the injured groin, i.e. crutch in right hand for a left groin injury) and then no crutches (see how to use crutches).
- Once symptoms settle, aim for pain free rehabilitation (i.e. gradually increase strength, flexibility and activity, provided there is no increase in symptoms during activity or upon rest following activity (i.e. the next morning). This should take place over a period of days to weeks, or, in some cases, months).
- Begin the “Initial Exercise” 72 hours following injury provided there is no increase in symptoms. A good indication that the exercise is helping is a reduction in pain directly after the exercise.
- Increase walking distance and eventually speed, gradually, and, provided there is no increase in pain or limp during or after the walk (this should take place over days to weeks, or, in some cases, months).
- Non-weight bearing, low impact or cross-training exercise may be performed to maintain cardiovascular fitness, such as swimming, water running, walking, the use of a cross trainer (elliptical trainer) or stationary exercise bike (in upright or standing positions) provided there is no increase in symptoms during or following the activity. Begin with a small duration of low intensity exercise and repeat every other day (i.e. 3 days per week). Aim to gradually increase the duration, intensity or frequency of training over a period of days, weeks or in some cases, months, provided there is no increase in symptoms.
- Progress to the “Intermediate Exercises” once your symptoms have settled consistently for a few days. The “Intermediate Exercises” should be added to the “Initial Exercise”. Generally you should select only one or two of the “Intermediate Exercises’ based on comfort and convenience. Ensure all new exercises do not increase symptoms. When performing the intermediate exercises, the ‘Initial Exercise’ can still be performed on alternate days (i.e. when you’re not performing the intermediate exercises).
- Progress to the “Advanced Exercises” once the “Intermediate Exercises” can be performed pain free and to the same extent on the injured side as the non-injured side. The “Advanced Exercises” should replace the “Intermediate Exercises” and can be added to the “Initial Exercises”. Generally you should select only one or two of the “Advanced Exercises’ based on comfort and convenience. Ensure all new exercises do not increase symptoms. When performing the advanced exercises, the ‘Initial Exercise’ can still be performed on alternate days (i.e. when you’re not performing the advanced exercises).
- The ‘Other Exercises’ may be required for those patients with residual hamstring tightness. These can be added once you can perform the advanced exercises without pain for a few days consecutively. Ensure there is no increase in symptoms. Generally you should begin with one of the exercises and then add the other after a few days provided there is no increase in pain.
- A gradual Return to Running Program should be implemented for individuals who aim to return to running following injury provided there is no increase in symptoms during and after activity with rest (i.e. the next night or morning).
- A gradual return to sport and activity can occur provided there is no increase in symptoms (see Return to Sport). Your physiotherapist can perform a Return to Sport Fitness test to assess whether you are ready to return to sport prior to doing so.
- Other Leg Stretches, Leg Strengthening Exercises and Balance Exercises may be added gradually (and provided symptoms do not increase) to improve flexibility, strength and control of the entire lower limb, to help prevent injury recurrence.
- Ensure your exercise regime, return to sport and general activity levels cause no increase in symptoms during or after activity throughout your rehabilitation.
- Ensure your physiotherapist has identified the contributing factors to your injury and appropriate intervention has taken place to address these issues to minimise the likelihood of injury recurrence.
 Find a Physio
Find a Physio
Find a physiotherapist in your local area who can treat hamstring origin tendonitis (tendinopathy).
 More Information
More Information
- Hamstring Strengthening Exercises.
- Resistance Band Exercises.
- Balance Exercises.
- How to use Crutches.
- R.I.C.E. Regime.
- Ice or Heat.
- Hamstring Stretches.
- Return to Running Program.
- Buttock Diagnosis Guide.
 Physiotherapy products
Physiotherapy products
Products that are commonly recommended to patients with hamstring origin tendonitis include:
To purchase these products either click on the appropriate link above or visit the PhysioAdvisor Shop.
+ 11 References
PhysioAdvisor relies on credible scientific sources (ideally from high quality randomised controlled trials, when available) to guide our content creation. Read about our sourcing guidelines and how we create trusted content via our editorial policy.
- Goom TS, Malliaras P, Reiman MP, Purdam CR. Proximal Hamstring Tendinopathy: Clinical Aspects of Assessment and Management. J Orthop Sports Phys Ther. 2016 Jun;46(6):483-93
- Jesus JF, Bryk FF, Moreira VC, Nakaoka GB, Reis AC, Lucareli PR. Gluteus Maximus inhibition in proximal hamstring tendinopathy.MedicalExpress. 2015 Aug;2(4)..
- Ebonie Rio; Dawson Kidgell; G Lorimer Moseley; Jamie Gaida; Sean Docking; Craig Purdam; Jill Cook, Changing the Way we Think About Tendon Rehabilitation A Narrative Review Br J Sports Med. 2016;50(4):209-215.
- Zissen MH, Wallace G, Stevens KJ, Fredericson M, Beaulieu CF. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. American Journal of Roentgenology. 2010 Oct;195(4):993-8.
- Brukner et al (2012). Brukner & Khan’s clinical sports medicine (4th ed.), 502-503. Australia: McGraw Hill Education.
- Cook JL1, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med. 2009 Jun;43(6):409-16.
- Cook JL, Purdam CR. The challenge of managing tendinopathy in competing athletes. Br J Sports Med. 2014 Apr;48(7):506-9.
- Beyer R, Kongsgaard M, Hougs Kjær B, Øhlenschlæger T, Kjær M, Magnusson SP. Heavy Slow Resistance Versus Eccentric Training as Treatment for Achilles Tendinopathy: A Randomized Controlled Trial. Am J Sports Med. 2015 Jul;43(7):1704-11.
- Korakakis V, Whiteley R, Tzavara A, et al The effectiveness of extracorporeal shockwave therapy in common lower limb conditions: a systematic review including quantification of patient-rated pain reduction Br J Sports Med 2018;52:387-407.
- Craig Purdam – What about hamstring tendinopathy?!Available from https://www.youtube.com/watch?v=FkOCoYq9iQQ
- Proximal Hamstring Tendinopathy – www.physio-pedia.com/Proximal_Hamstring_Tendinopathy
Become a PhysioAdvisor Member
-
 Individual Membership (12 Months)$59.95 for 1 year
Individual Membership (12 Months)$59.95 for 1 year -
 Individual Membership (3 Months)$39.95 for 3 months
Individual Membership (3 Months)$39.95 for 3 months -
 Individual Membership (Yearly)$49.95 / year
Individual Membership (Yearly)$49.95 / year -
 Individual Membership (Monthly)$15.95 / month
Individual Membership (Monthly)$15.95 / month

Link to this Page
If you would like to link to this article on your website, simply copy the code below and add it to your page:
<a href="https://physioadvisor.com.au/injuries/buttock/hamstring-origin-tendonitis”>Hamstring Origin Tendonitis (Tendinopathy) – PhysioAdvisor.com</a><br/>Expert physiotherapy information on hamstring origin tendonitis (tendinopathy) including symptoms, causes, comprehensive treatment, exercises & rehab guide.
Return to the top of Hamstring Origin Tendonitis (Tendinopathy).






