Patellofemoral Pain Syndrome
Updated:
(Also known as PFPS, Patellofemoral Syndrome, Patellofemoral Joint Syndrome, PFJ Syndrome, Chondromalacia Patellae, Anterior Knee Pain, Patella Pain Syndrome, Runner’s Knee)
What is patellofemoral pain syndrome?
Patellofemoral pain syndrome is the term given to pain originating from the patellofemoral joint (i.e. the joint between the knee cap (patella) and thigh bone (femur)) usually as a result of inflammation or tissue damage to structures of the patellofemoral joint.
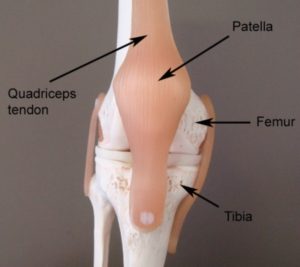
The knee comprises of the union of 3 bones – the long bone of the thigh (femur), the shin bone (tibia) and the knee cap (patella) (figure 1). The patella (knee cap) is situated at the front of the knee and lies within the tendon of the quadriceps muscle (the muscle at the front of the thigh). The quadriceps tendon envelops the patella and attaches to the top end of the tibia (figure 1). Due to this relationship, the knee cap sits in front of the femur forming a joint in which the bones are almost in contact with each other. The surface of each bone, however, is lined with cartilage to allow cushioning between the bones. This joint is called the patellofemoral joint.
Normally, the patella is aligned in the middle of the patellofemoral joint so that forces applied to the knee cap during activity are evenly distributed. In patients with patellofemoral pain syndrome the patella is often misaligned relative to the femur, which therefore places more stress through the patellofemoral joint during activity. These biomechanical anomalies can predispose the joint to injury. This may particularly be so, during activities that place repetitive, prolonged or traumatic force on the patellofemoral joint. When these forces are beyond what the joint can withstand, damage and inflammation to structures of the patellofemoral joint (such as cartilage, or connective tissue) may occur, with subsequent patellofemoral pain. This condition is known as patellofemoral pain syndrome.
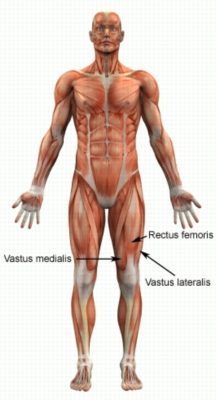
Patella misalignment (which is often present in patients with patellofemoral pain syndrome) may occur for various reasons. One of the main causes is an imbalance in strength between two parts of the quadriceps muscle. The quadriceps muscle comprises of 4 muscle bellies, 2 lie centrally (rectus femoris and vastus intermedius), one lies on the inner leg (vastus medialis) and one lies on the outer leg (vastus lateralis) (figure 2). In the majority of patellofemoral pain syndrome cases, the outer quadriceps (vastus lateralis) is stronger than the inner quadriceps (vastus medialis), resulting in the knee cap being pulled towards the outside of the leg. This may result in abnormal movement of the knee cap when bending and straightening the knee. There are numerous factors which can cause this strength imbalance of the quadriceps (such as abnormal lower limb biomechanics, pain inhibition etc.). These need to be identified and corrected by a physiotherapist.
Patellofemoral pain syndrome is a very common condition that is frequently seen in clinical practice, particularly in runners. It often affects adolescents at a time of increased growth and usually affects girls more than boys. In older patients, patellofemoral pain syndrome is often associated with degenerative joint changes.
Signs and symptoms of patellofemoral pain syndrome
Patients with patellofemoral pain syndrome usually experience pain at the front of the knee and around or under the knee cap. Pain can sometimes be felt at the back of the knee or on the inner or outer aspects. Patients usually experience an ache that may increase to a sharper pain with activity.
In less severe cases, patients may only experience an ache or stiffness in the knee that increases with rest (typically at night or first thing in the morning) following activities that place stress on the patellofemoral joint. These activities typically include excessive standing or walking (especially up and down stairs or hills or on uneven surfaces), heavy lifting (particularly with knees bent), deep squatting, lunging, kneeling, running, hopping, jumping, twisting or other activities that bend and straighten the knee during weight bearing. The pain associated with this condition may also warm up with activity in the initial stages of injury. As the condition progresses, patients may experience symptoms that increase during sport or activity, affecting performance. Symptoms typically increase on firmly touching the margins of the patellofemoral joint.
Occasionally, patients with this condition may experience pain whilst sitting or driving with the knee bent for prolonged periods. There may also be an associated clicking or grinding sound when bending or straightening the knee. In more severe cases, patients may walk with a limp and sometimes may experience episodes of the knee giving way or collapsing due to pain. In chronic cases there may be evidence of quadriceps muscle wasting (particularly of the vastus medialis – figure 2).
Diagnosis of patellofemoral pain syndrome
A thorough subjective and objective examination from a physiotherapist is usually sufficient to diagnose patellofemoral pain syndrome. Investigations such as an X-ray or MRI may be used to assist with diagnosis.
Prognosis of patellofemoral pain syndrome
Most patients with this condition heal well with appropriate physiotherapy management and return to normal function in a number of weeks. Occasionally, rehabilitation can take significantly longer and may take many months in those who do not follow appropriate rehabilitation instructions correctly. Even patients who have had their condition for a long period of time can usually make marked improvements in a short period of time with appropriate physiotherapy management. Early physiotherapy treatment is vital to hasten recovery in all patients with this condition.
Treatment for patellofemoral pain syndrome

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Contributing factors to the development of patellofemoral pain syndrome
There are several factors which can predispose patients to developing patellofemoral pain syndrome. These need to be assessed and corrected with direction from a physiotherapist. Some of these factors include:
- muscle strength imbalances
- muscle weakness (especially the VMO and gluteal muscles)
- tightness in specific joints (hip, knee or ankle)
- tightness in specific muscles (especially the ITB or quadriceps)
- excessive or inappropriate training or activity
- inadequate recovery periods from training or activity
- inappropriate footwear or training surfaces
- poor training technique
- a shallow femoral groove (i.e. the groove that the knee cap sits within)
- genu valgum (‘knock knees’)
- femoral anteversion (where the thigh bones turn inward)
- patella alta (abnormally high patella in relation to the thigh bone)
- increased femoral internal rotation (inward turning of the thigh bone)
- poor lower limb or foot biomechanics (e.g. flat feet, high arches or increased Q angle)
- general hypermobility
- poor balance
- poor pelvic or core stability
- poor landing strategies
- poor coordination
- gender (i.e. greater likelihood in females)
- a current or past lower limb injury (particularly the knee) that has been poorly rehabilitated
Physiotherapy for patellofemoral pain syndrome
Physiotherapy treatment and rehabilitation for patellofemoral pain syndrome is vital to hasten the healing process and ensure an optimal outcome. Treatment may comprise:
- soft tissue massage
- electrotherapy
- the use of crutches
- patella taping or bracing to correct patella position
- foot taping to improve foot posture and biomechanics
- joint mobilization
- dry needling
- ice or heat treatment
- progressive exercises to improve flexibility, balance and strength (especially the VMO muscle)
- activity modification advice
- biomechanical correction (e.g. the prescription of orthotics)
- anti-inflammatory advice
- weight loss advice where appropriate
- the use of Real-Time Ultrasound to assess and retrain the VMO muscle
- education
- a graduated return to activity program
Other intervention for patellofemoral pain syndrome
Despite appropriate physiotherapy management, a small percentage of patients with patellofemoral pain syndrome do not improve adequately. When this occurs the treating physiotherapist or doctor can advise on the best course of management. This may include pharmaceutical intervention, corticosteroid injection, further investigation such as an X-ray, MRI or CT Scan or a referral to a sports doctor or orthopaedic specialist who will advise on any procedures that may be appropriate to improve the condition. A review with a podiatrist may also be indicated for the prescription of orthotics to correct any foot posture abnormalities.
Exercises for patellofemoral pain syndrome
The following exercises are commonly prescribed to patients with this condition. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 2 – 3 times daily and only provided they do not cause or increase symptoms.
Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate, advanced and other exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms.
Initial Exercises
Static Quadriceps Contraction
Tighten the muscle at the front of your thigh (quadriceps) by pushing your knee down into a towel (figure 3). Put your fingers on your inner quadriceps (vastus medialis – figure 2) to feel the muscle tighten during contraction. Hold for 5 seconds and repeat 10 times as hard as possible without increasing your symptoms.

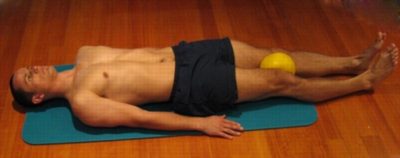
Adductor Squeeze (Supine)
Begin this exercise lying on your back in the position demonstrated with a Pilates ball or rolled towel between your knees (figure 4). Tighten your thigh muscles (quadriceps) by straightening your knees and then slowly squeeze the ball between your knees tightening your inner thigh muscles (adductors). Hold for 5 seconds and repeat 10 times as hard as possible and comfortable provided the exercise is pain free.
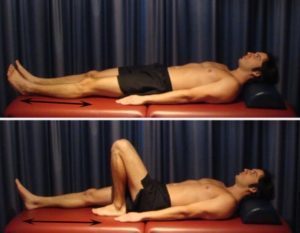
Knee Bend to Straighten
Bend and straighten your knee as far as you can go without pain and provided you feel no more than a mild to moderate stretch (figure 5). Gradually increase movement as tolerated provided the exercise is pain free. Repeat 5 – 15 times provided there is no increase in symptoms.
Hip Extension in Standing
Begin this exercise standing at a table or bench for balance. Keeping your back and knee straight, slowly take your leg backwards, tightening your bottom muscles (gluteals) (figure 6). Hold for 2 seconds then slowly return to the starting position. Repeat 10 times provided the exercise is pain free.

Intermediate Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Advanced Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Other Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Rehabilitation guide for patellofemoral pain syndrome

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
 Find a Physio for patellofemoral pain syndrome
Find a Physio for patellofemoral pain syndrome
Find a Physiotherapist in your local area who can treat patellofemoral pain syndrome.
 More Exercises
More Exercises
- Knee Strengthening Exercises.
- Knee Flexibility Exercises.
- Balance Exercises.
- Leg Stretches.
- Leg Strengthening Exercises.
- Lower Body Foam Roller Exercises
- Lower Body Massage Ball Exercises
 Physiotherapy products
Physiotherapy products
Some of the most commonly recommended products by physiotherapists to hasten healing and speed recovery in patients with patellofemoral pain syndrome include:
To purchase physiotherapy products for patellofemoral pain syndrome click on one of the above links or visit the PhysioAdvisor Shop.
 More Information
More Information
- R.I.C.E. Regime.
- How to use Crutches.
- Do I Need Orthotics?
- Foot Taping.
- Ice or Heat.
- Return to Running Program.
- Return to Sport.
- Patella Taping.
- Why is my Injury not Improving?
- Knee Diagnosis Guide.
Become a PhysioAdvisor Member
+ 14 References
PhysioAdvisor relies on credible scientific sources (ideally from high quality, randomised controlled trials, where available) to guide our content creation. Read about our sourcing guidelines and how we create trusted content via our editorial policy.
- Barton CJ, Lack S,Hemmings S, et al. The ‘Best practice guide to conservative management of patellofemoral pain’: incorporating level 1 evidence with expert clinical reasoning. Br J Sports Med 2015;49:923–34. doi:10.1136/bjsports-2014-093637
- Brukner et al (2012). Brukner & Khan’s clinical sports medicine (4th ed.), 689. Australia: McGraw Hill Education.
- Wood L, Muller S, Peat G. The epidemiology of patellofemoral disorders in adulthood: a review of routine general practice morbidity recording. Prim Health Care Res Dev 2011;12:157–64. doi:10.1017/S1463423610000460
- van Middelkoop M, van Linschoten R, Berger MY, et al. Knee complaints seen in general practice: active sport participants versus non-sport participants. BMC Musculoskelet Disord 2008;9:36. doi:10.1186/1471-2474-9-36
- Lankhorst NE, van Middelkoop M, Crossley K, et al. Factors that predict a poor outcome 5–8 years after the diagnosis of patellofemoral pain: a multicentre observational analysis. Br J Sports Med 2016;50:881–86. doi:10.1136/bjsports-2015-094664
- Collins NJ, Bierma-Zeinstra SM, Crossley KM, et al. Prognostic factors for patellofemoral pain: a multicentre observational analysis. Br J Sports Med 2013;47:227–33. doi:10.1136/bjsports-2012-091696
- Rathleff MS, Rathleff CR,Olsen JL, et al. Is knee pain during adolescence a self-limiting condition?: prognosis of patellofemoral pain and other types of knee pain. Am J Sports Med 2016;44:1165–71. doi:10.1177/0363546515622456
- Boling M, Padua D, Marshall S, et al. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports 2010;20:725–30. doi:10.1111/j.1600-0838.2009.00996.x
- Bolgla LA, Boling MC. An update for the conservative management of patellofemoral pain syndrome: a systematic review of the literature from 2000 to 2010. Int J Sports Phys Ther 2011;6:112–25.
- Clijsen R, Fuchs J,Taeymans J. Effectiveness of exercise therapy in treatment of patients with patellofemoral pain syndrome: systematic review and meta-analysis. Phys Ther 2014;94:1697–708. doi:10.2522/ptj.20130310
- Collins NJ, Bisset LM,Crossley KM, et al. Efficacy of nonsurgical interventions for anterior knee pain systematic review and meta-analysis of randomized trials. Sports Med 2012;42:31–49. doi:10.2165/11594460-000000000-00000
- Patellofemoral Pain Syndrome (2015), www.orthoinfo.aaos.org/en/diseases–conditions/patellofemoral-pain-syndrome/
- Patellofemoral Pain Syndrome (Knee Cap Pain) (2017), www.mydr.com.au/sports-fitness/patellofemoral-pain-syndrome-kneecap-pain/
- Patellofemoral Pain Syndrome, www.physio-pedia.com/Patellofemoral_Pain_Syndrome

Link to this Page
If you would like to link to this article on your website, simply copy the code below and add it to your page:
<a href="https://physioadvisor.com.au/injuries/knee/patellofemoral-pain-syndrome”>Patellofemoral Pain Syndrome – PhysioAdvisor.com</a><br/>Get detailed information on Patellofemoral Pain Syndrome - causes, signs and symptoms, diagnosis, treatment, exercises, physiotherapy products and more.
Return to the top of Patellofemoral Pain Syndrome.











