Adductor Tendonitis (Tendinopathy)
Updated:
(Also known as Adductor Tendinopathy, Adductor Tendinitis, Adductor Tendinosis, Groin Tendonitis, Groin Tendinopathy, Groin Tendinitis, Groin Tendinosis)
N.B. Although recent research suggests that ‘adductor tendinopathy’ is the more appropriate term to describe overuse injuries to the adductor tendon (due to the absense of an inflammatory response), we will use the term ‘adductor tendonitis’ in this document as it is more widely known.
What is adductor tendonitis?
Adductor tendonitis is a condition characterised by tissue damage, degeneration and sometimes swelling to the adductor tendon at its attachment to the pelvis resulting in groin pain.
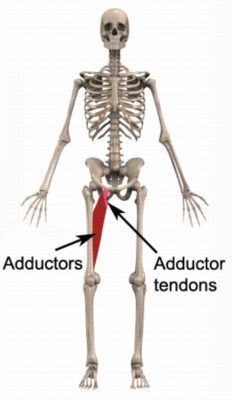
The muscles at the inner aspect of your thigh are known as the adductor muscles (groin). These muscles (i.e. the adductor magnis, adductor longus, adductor brevis and gracilis) originate from the pelvis and insert into the inner aspect of the thigh bone (femur) and lower leg bone (tibia) (figure 1). The adductor muscles attach to their bony origin and insertion via their respective adductor tendons.
The adductor muscles are responsible for stabilising the pelvis and moving the leg towards the midline of the body (adduction). They are particularly active during running (especially when changing direction) and kicking.
During contraction and stretch of the groin muscles, tensile and compression forces are placed through the adductor tendons at their attachment to the pelvis. When these forces are excessive due to too much repetition, prolonged or high force, damage to one or more of the adductor tendons may occur.
Adductor tendonitis (tendinopathy) is a condition comprising damage to the respective adductor tendon with subsequent degeneration and disorganisation of collagen fibres (a protein giving the tendon its tensile strength). This may also be accompanied by swelling or thickening of the tendon. These changes impair the tendon’s ability to withstand stress.
3 Phases of Adductor Tendonitis (Tendinopathy)
Due to the tendons inability to adapt appropriately to an increase in load on the tendon, adductor tendonitis (tendinopathy) may progress through 3 different phases:
- Reactive Phase – This involves a short term adaptation to stress, that thickens the tendon, reduces stress and increases tendon stiffness. During this phase, changes to the tendon are typically reversible (with appropriate management) and the tendon remains structurally intact.
- Dysrepair Phase – This phase follows the reactive phase if the tendon continues to be loaded excessively. It is characterised by changes and breakdown in the tendon structure. In addition, new blood vessels and nerves begin to grow resulting in an increase in tendon sensitivity / pain. Appropriate treatment is vital during this phase to prevent progression to the degenerative phase.
- Degenerative Phase – This phase represents changes to chronic tendon overload. Further changes and breakdown in the tendon structure occur. Collagen becomes disorganised. Further growth of new blood vessels and nerves occurs. Areas of cell death occur. The tendon may appear thickened or nodular and be at a higher risk or rupture.
Causes of adductor tendonitis
Adductor tendonitis is usually an overuse injury, which commonly occurs due to repetitive or prolonged activities placing strain on the adductor tendon. This typically occurs due to repetitive running, kicking or change of direction activities.
Occasionally, patients may develop this condition suddenly due to a forceful contraction of the adductor muscles often when they are in a position of stretch. This typically occurs during rapid acceleration whilst running (particularly when changing direction) or when a footballer performs a long kick.
Adductor tendonitis is commonly seen in running sports such as football, hockey and athletics (particularly sprinters, hurdlers, and long jumpers) as well as in skiing, horse riding and gymnastics.
Patients may also develop this condition following inappropriate or inadequate treatment of an acute groin strain.
Signs and symptoms of adductor tendonitis
Patients with this condition typically experience groin pain that develops gradually overtime. Patients usually experience pain on firmly touching the adductor tendon at its attachment to the pelvis (figure 1). Pain may also increase when squeezing the legs together or when moving the affected leg away from the midline of the body (i.e. abduction, for example, when performing a groin stretch).
In less severe cases, patients may only experience an ache or stiffness in the groin that increases with rest following activities requiring strong, repetitive or prolonged contraction or stretch of the adductor muscles. These activities typically include running, kicking and change of direction activities. The pain associated with this condition may also warm up with activity in the initial stages of the condition.
As the condition progresses, patients may experience symptoms that increase during activity and affect performance. In severe cases of adductor tendonitis (tendinopathy) the patient may be unable to continue the activity and may limp as a result of pain.
Diagnosis of adductor tendonitis
A thorough subjective and objective examination from a physiotherapist is usually sufficient to diagnose adductor tendonitis. Further investigations such as an X-ray, ultrasound, MRI or CT scan may be required occasionally, to confirm diagnosis, assess the severity of the injury and rule out other conditions.
Treatment for adductor tendonitis

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Prognosis of adductor tendonitis
Most patients with adductor tendonitis heal well with appropriate physiotherapy and return to normal function in a number of weeks (particularly those in the acute reactive phase of the condition). For those patients who progress to the dysrepair or degenerative phase, rehabilitation can take significantly longer and may take many months to optimise recovery (particularly in those who have had their condition for a long period of time). For patients with a degenerative adductor tendonitis (tendinopathy), there is a significantly increased risk of a sub-optimal outcome. Early physiotherapy treatment is vital to hasten recovery in all patients with this condition and prevent injury progression.
Contributing factors to the development of adductor tendonitis
There are several factors which can predispose patients to developing this condition. These need to be assessed and corrected with direction from a physiotherapist. Some of these factors include:
- muscle tightness (particularly of the adductors, gluteals, hip flexors, or hamstrings)
- poor biomechanics
- muscle weakness (especially of the groin, gluteals or core stabilisers)
- inadequate rehabilitation following a previous adductor injury
- inappropriate or excessive training or activity
- inadequate recovery periods from sport or activity
- change in training conditions or surfaces
- poor posture
- poor foot posture (e.g. flat feet)
- inappropriate footwear
- inappropriate running technique
- inadequate fitness
- fatigue
- inadequate warm up
- joint stiffness (particularly the lower back, hip and knee)
- poor pelvic and core stability
- neural tightness
- muscle imbalances
- being overweight
Physiotherapy for adductor tendonitis
Physiotherapy for patients with adductor tendonitis is vital to hasten the healing process, ensure an optimal outcome and reduce the likelihood of future recurrence. Treatment may comprise:
- soft tissue massage (particularly to the adductors and abductors)
- electrotherapy (e.g. ultrasound)
- muscle energy techniques
- joint mobilization (in particular the lumbar spine and hip joint)
- ice or heat treatment
- the use of a compression bandage or strapping
- education
- biomechanical correction
- the use of crutches
- dry needling
- progressive exercises to improve strength, flexibility, core stability, pelvic stability and balance
- clinical Pilates
- hydrotherapy
- activity modification advice
- technique correction
- anti-inflammatory advice
- prescription of orthotics
- footwear advice
- devising and monitoring a return to sport or activity plan
Other intervention for adductor tendonitis
Despite appropriate physiotherapy management, some patients with this condition do not improve adequately. When this occurs, the treating physiotherapist or doctor can advise on the best course of management. This may include investigations such as an X-ray, ultrasound, CT scan or MRI, pharmaceutical intervention, corticosteroid injection, autologous blood injection or referral to appropriate medical authorities who can advise on any intervention that may be appropriate to improve the condition. A review with a podiatrist may be indicated for the prescription of orthotics in patients with abnormal foot biomechanics. In very rare cases surgical intervention may be considered.
Exercises for adductor tendonitis
The following exercises are commonly prescribed to patients with adductor tendonitis. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 3 times daily and only provided they do not cause or increase symptoms.
Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate and advanced exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place gradually and provided there is no increase in symptoms.
Initial Exercises
Adductor Squeeze (Crook Lying)
Begin this exercise lying in the position demonstrated with a rolled towel or ball between your knees (figure 2). Slowly squeeze the ball between your knees tightening your inner thigh muscles (adductors). Hold for 5 – 10 seconds and repeat 5 times at an intensity that is comfortable and does not cause pain. Allow an equal period of time to rest between each repetition (i.e. 5 seconds rest for a 5 second contraction). Once this is easy, you can gradually build up the intensity of contraction and duration of contraction (slowly over a number of days) to as long as 45 second holds (with 45 seconds rest between repetitions), provided there is no increase in symptoms.

Adductor Squeeze (Supine)
Begin this groin strengthening exercise lying on your back in the position demonstrated with a rolled towel or ball between your knees (figure 3). Slowly squeeze the ball between your knees tightening your inner thigh muscles (adductors). Hold for 5 – 10 seconds and repeat 5 times at an intensity that is comfortable and does not cause pain. Allow an equal period of time to rest between each repetition (i.e. 5 seconds rest for a 5 second contraction). Once this is easy, you can gradually build up the intensity of contraction and duration of contraction (slowly over a number of days) to as long as 45 second holds (with 45 seconds rest between repetitions), provided there is no increase in symptoms.

Hip Abduction
Begin this exercise lying on your back (figure 4). Keeping your knee straight, take your leg to the side as far as you can go without pain and provided you feel no more than a mild stretch, then return to the starting position. Begin with no further than 50 – 75% of your available range of movement (to avoid excessive tensile and compression stress on the adductor tendon). Slowly build up to 100% of your available movement over a number of days provided there is no increase in symptoms. Keep your knee cap and toes facing the ceiling throughout the exercise. Repeat 5 – 15 times provided there is no increase in symptoms.

Intermediate Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Advanced Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Rehabilitation Protocol for adductor tendonitis

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
 Find a Physio
Find a Physio
Find a physiotherapist in your local area who can treat adductor tendonitis (tendinopathy).
 Physiotherapy products for adductor tendonitis
Physiotherapy products for adductor tendonitis
The most commonly recommended products by physiotherapists to hasten healing and speed recovery in patients with this condition include:
To purchase physiotherapy products for adductor tendonitis click on one of the above links or visit the PhysioAdvisor Shop.
 Other Exercises
Other Exercises
- Hip Strengthening Exercises.
- Leg Strengthening Exercises
- Groin Stretches.
- Leg Stretches
- Balance Exercises
- Beginner Pilates Exercises to improve core stability and posture.
 More information
More information
- Learn How to Use Crutches
- View detailed information on when to use Ice or Heat
- Read about initial injury management and the R.I.C.E. Regime.
- View detailed information on Do I Need Orthotics?
- Read about PhysioAdvisor’s Return to Running Program.
- Learn about safely Returning to Sport.
- Read our Hip & Groin Diagnosis Guide.
Become a PhysioAdvisor Member
+ 7 References
PhysioAdvisor relies on credible scientific sources (ideally from high quality randomised controlled trials, when available) to guide our content creation. Read about our sourcing guidelines and how we create trusted content via our editorial policy.
- Khan KM, Cook JL, Bonar F, Harcourt P, Astrom M. Histopathology of common tendinopathies. Update and implications for clinical management. Sports Med. 1999;27:393–408
- Ebonie Rio; Dawson Kidgell; G Lorimer Moseley; Jamie Gaida; Sean Docking; Craig Purdam; Jill Cook, Changing the Way we Think About Tendon Rehabilitation A Narrative Review Br J Sports Med. 2016;50(4):209-215.
- Brukner et al (2012). Brukner & Khan’s clinical sports medicine (4th ed.), 559. Australia: McGraw Hill Education.
- Cook JL1, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med. 2009 Jun;43(6):409-16.
- Holmich P, Uhrskou P, Ulnits L, et al: Effectiveness of active physical training as treatment for long-standing adductor-related groin pain in athletes: Randomised trial. Lancet 353: 439-443, 1999
- Adductor Tendonitis (2019) – physioworks.com.au/injuries-conditions-1/adductor-tendinopathy
- Adductor Tendinopathy – www.physio-pedia.com/Adductor_Tendinopathy

Link to this Page
If you would like to link to this article on your website, simply copy the code below and add it to your page:
<a href="https://physioadvisor.com.au/injuries/hip-groin/adductor-tendonitis”>Adductor Tendonitis (Tendinopathy) – PhysioAdvisor.com</a><br/>Expert physiotherapy information on adductor tendonitis (tendinopathy) including: diagnosis, treatment, exercises, rehab protocol, physio products and more
Return to the top of Adductor Tendonitis (Tendinopathy).











