Femoroacetabular Impingement (FAI)
Updated:
(Also known as FAI, Hip Impingement)
What is femoroacetabular impingement?
Femoroacetabular impingement (FAI) is a condition involving increased bony growth of one or both bones that form the ball and socket joint of the hip. This irregular bony growth results in a mechanical incongruity which predisposes the joint to premature contact between the bones during activity.
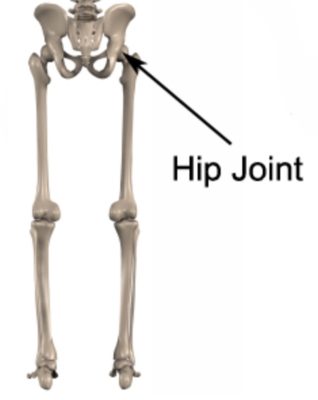
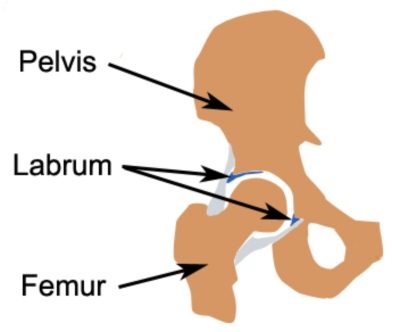
Relevant anatomy for femoroacetabular impingement
The ball and socket joint of the hip is formed from the union of two bones: The top of the thigh bone (i.e. femur giving rise to the ball) and the pelvis (giving rise to the socket). The depth of the socket of the hip joint is increased by strong cartilage known as the labrum which attaches to the rim of the hip joint (figures 1 & 2).The labrum increases the depth of the socket and aids shock absorption. Articular cartilage also lines the ball (femoral head) and socket (acetabulum) further improving joint shock absorption by cushioning the impact of the ball on the socket during weight bearing activity. Strong connective tissue known as the joint capsule and ligaments hold the bones together.
Types of femoroacetabular impingement
There are 3 types of femoroacetabular impingement: cam, pincer and combined impingement:
Cam FAI
Cam femoroacetabular impingement involves the formation of a bump right next to the edge of the ball of the hip joint (i.e. at the femoral head / neck junction). This causes the ball to lose its optimal spherical shape. Subsequently, earlier compression of the ball and socket joint may occur during activity. Cam FAI is more common in athletic males.
Pincer FAI
Pincer femoroacetabular impingement occurs when bony growth at the edges of the socket increases its depth (i.e. the acetabular rim). This causes the edge of the socket to impact the ball and adjacent tissue (such as the labrum and articular cartilage) during certain movements. Pincer FAI is more common in women.
Combined FAI
Combined FAI occurs when both Cam and Pincer abnormalities are present simultaneously.
It is important to note that Cam and Pincer abnormalities are relatively common in people without symptoms, occurring in around 30% of the general population. Therefore, the presence of these changes alone are not sufficient to form a femoroacetabular impingement diagnosis (see Diagnosis below for more information).
Cause of femoroacetabular impingement
According to a systematic review by Chaudhry and Aveni (2014), the cause of femoroacetabular impingement is likely to be due to a number of factors. These may include:
- Sex – There is a higher incidence of cam abnormalities in males and pincer morphology in females.
- Family history – patients with FAI are more likely to have siblings with similar findings on X-Ray.
- Exposure to repetitive (and often excessive) hip rotation and flexion during childhood or adolescence (e.g. hockey, basketball or football). It is thought that these stresses may cause adaptive bone remodelling with subsequent development of FAI abnormalities.
- History of childhood hip disease resulting in alteration of the normal shape of the femoral head (e.g. Slipped Upper Femoral Epiphysis (SUFE) or Perthes disease).
- Surgical over-correction of hip dysplasia may lead to pincer abnormality
- Malunion of fractures affecting the femoral neck. This may alter the normal shape of the bone leading to FAI.
Cause of Symptoms
Once the mechanical changes of femoroacetabular impingement have been established (i.e. cam, pincer or combined abnormalities), patients are more likely to become symptomatic during activities causing increased compression between the bones of the hip. This may occur during activities or sports involving repetitive, prolonged or forceful:
- Twisting
- Change of direction
- Weight bearing
- End of range hip movement (particularly flexion and rotation).
Some sports involving an increased incidence of FAI may include:
- Football
- Soccer
- Tennis
- Basketball
- Hockey
- Dancing (e.g. Ballet)
- Martial Arts
- Water Polo
Symptoms may also develop during running or due to direct trauma such as a fall, heavy landing, heavy lifting (especially whilst twisting) or motor vehicle accident.
Patients may also develop their symptoms gradually over time due to overuse. This may be due to excessive twisting or weight bearing activity over time (e.g. long distance walking or running, especially on uneven surfaces or up or down hills or stairs), repetitive squatting or lunging, or, excessive kicking (e.g. in football, dancing or martial arts). In older patients, degenerative changes to the hip joint may also be present. In these instances, symptom onset may occur with a trivial incident.
Signs and symptoms of femoroacetabular impingement
Patients with this condition usually experience pain in the hip or groin. This may be combined with pain in the buttock, pelvic region, lower back or thigh. Symptom exacerbation usually occurs with excessive weight bearing activity (e.g. excessive walking, running, carrying, lifting or jumping) and twisting movements of the hip. Patients may also experience pain when kicking, squatting or lunging, when climbing stairs, getting in and out of the car (or bed) or when lying on the affected side.
Other symptoms may include:
- Hip stiffness
- Loss of hip flexibility / range of movement
- A feeling of weakness in the hip
- Clicking, locking or giving way of the hip
- Catching pains
- Difficulty weight bearing
- An observable limp
Diagnosis of femoroacetabular impingement
A diagnosis of FAI usually requires a triad of findings (Griffin et al 2016) including:
- Symptoms associated with femoroacetabular impingement (FAI) such as hip or groin pain.
- Radiological or imaging findings such as cam or pincer morphology or soft tissue findings.
- Signs of FAI on objective clinical testing – such as a positive FADIR test, muscle weakness, hip stiffness, poor functional performance.
Subsequently, a thorough subjective and objective examination from a physiotherapist combined with radiological changes on X-Ray, CT scan or MRI are usually required to diagnose femoroacetabular impingement. Radiological investigations may also be helpful determining the presence of other co-existing injuries.
Treatment for femoroacetabular impingement

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Surgery for femoroacetabular impingement

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Contributing factors to the development of femoroacetabular impingement
There are a variety of factors which may contribute to the onset of FAI. These need to be assessed and, where possible, corrected with direction from a physiotherapist. Some of these factors include:
- Exposure to repetitive (and often excessive) hip rotation and flexion during childhood or adolescence (e.g. hockey, basketball or football).
- Sex – males having more cam abnormalities, females having more pincer morphology.
- Family history (particularly siblings)
- History of childhood hip diseases (such as Perthes or SUFE) altering the normal shape of the femoral head.
- Surgical over-correction of hip dysplasia
- Malunion of femoral neck fractures.
- Inappropriate or excessive training or activity
- Inadequate recovery periods from sport or activity
- Muscle weakness (particularly the gluteals)
- Muscle tightness (particularly the gluteals or hip flexor muscles)
- Joint stiffness (particularly of the hip)
- Inappropriate running technique
- Training on inappropriate surfaces (particularly hard, uneven or cambered surfaces)
- Leg length discrepancy
- Poor foot bio-mechanics
- Inappropriate footwear
- Inadequate rehabilitation following a previous hip or lower limb injury
- Insufficient warm up
- Being overweight
- Poor core stability
- Poor balance
Physiotherapy for femoroacetabular impingement
Physiotherapy treatment should be the first line of treatment for all patients with femoroacetabular impingement. Physiotherapy can hasten the healing process, correct identified impairments and assist with optimising the outcome in all patients with femoroacetabular impingement (regardless of whether they have surgery). Treatment may comprise:
- education
- soft tissue massage
- dry needling
- electrotherapy
- joint mobilization
- stretches
- hydrotherapy
- the use of crutches
- ice or heat treatment
- bio-mechanical correction (e.g. the use of orthotics)
- activity modification and pacing advice
- anti-inflammatory advice
- weight loss advice where appropriate
- progressive exercises to improve flexibility, balance and strength
- Clinical Pilates
- a gradual return to running program
- a gradual return to sport or activity program
For those patients who are surgical candidates, physiotherapy and rehabilitation should begin prior to surgery. This may include treatment to reduce pain, swelling and inflammation, improve flexibility, strength and function and to correct bio-mechanics. Following surgery, physiotherapy and rehabilitation is essential to assist the healing process and ensure an optimal outcome.
Prognosis of femoroacetabular impingement
Most patients with minor to moderate femoroacetabular impingement (and a significant portion of those with severe FAI) can expect good to great outcomes with appropriate conservative management. Return to sport or activity can often occur in approximately 2 – 8 weeks.
For patients who are managed surgically, quality of life scores typically improve, however patients will still usually have impairment compared to age matched individuals. Sometimes return to sport or activity may occur within 8 weeks, although most patients (especially when the FAI is moderate to severe) will require a significantly longer rehabilitation period.
It is important that FAI injuries are managed appropriately to minimise the risk of developing early hip osteoarthritis.
Other intervention for femoroacetabular impingement
Despite appropriate physiotherapy treatment and rehabilitation, some patients with FAI do not improve sufficiently either conservatively or following surgery. In these cases, the treating physiotherapist or doctor can advise on the best course of management. This may entail additional investigations such as X-rays, ultrasound, CT scan or MRI, pharmaceutical intervention, corticosteroid injection, or further surgery.
Exercises for femoroacetabular impingement
The following exercises are commonly prescribed to patients with this condition. The suitability of these exercises should be discussed with your physiotherapist prior to commencement. Generally, they should be performed 3 times daily provided they do not cause or increase symptoms.
Your physiotherapist can advise when to begin the initial exercises and progress to the intermediate and advanced exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms.
Initial Exercises
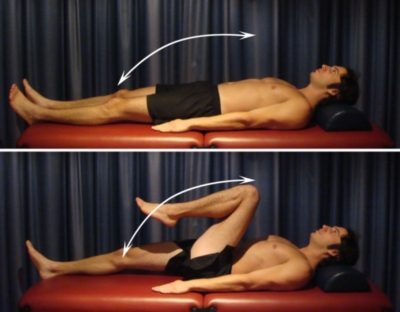
Hip Abduction
Begin lying on your back on a bed (figure 3). Keeping your knee straight (and your heel in contact with the bed – if the bed is large enough), take your leg to the side as far as you can go without pain and provided you feel no more than a mild to moderate stretch, then return to the starting position. Keep your knee cap and toes facing the ceiling and allow the bed to take the weight of your leg throughout the exercise. Repeat 5 – 15 times provided there is no increase in symptoms.

Hip External Rotation
Start this exercise lying on your back with your knee bent and foot flat on the floor (figure 4). Take your knee to the side as far as you can go without pain and provided you feel no more than a mild to moderate stretch, then return to the starting position. Repeat 5 – 15 times provided there is no increase in symptoms.

Hip Extension in Lying
Begin this exercise lying on your stomach in the position demonstrated (figure 5). Keeping your knee straight, slowly lift your leg tightening your bottom muscles (gluteals). Hold for 2 seconds and repeat 5 – 10 times provided the exercise is pain free.

Hip Flexion
Begin this exercise lying on your back (figure 6). Slowly take your knee to your chest as far as you can go without pain and provided you feel no more than a mild to moderate stretch, then lower back down. Repeat 5 – 10 times provided there is no increase in symptoms. (N.B. If this exercise is too uncomfortable initially, a gentler alternative is to bring your knee towards your chest whilst keeping your foot / heel in contact with the bed. Slowly slide your heel towards your bottom as far as you can go without pain and provided you feel no more than a mild to moderate stretch, then lower back down.)
Intermediate Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Advanced Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Other Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Rehabilitation Protocol for femoroacetabular impingement

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
 Physiotherapy products for femoroacetabular impingement
Physiotherapy products for femoroacetabular impingement
Some of the most commonly recommended products by physiotherapists to hasten healing and speed recovery in patients with this condition include:
To purchase physiotherapy products for femoroacetabular impingement click on one of the above links or visit the PhysioAdvisor Shop.
 Find a Physio for femoroacetabular impingement
Find a Physio for femoroacetabular impingement
Find a physiotherapist in your local area who can treat femoroacetabular impingement.
 Other exercises
Other exercises
- Hip Flexibility Exercises.
- Hip Strengthening Exercises.
- Core Stability Exercises
- Balance Exercises
- Beginner Pilates Exercises to improve core stability and posture.
 More information
More information
- How to use Crutches.
- Ice or Heat.
- R.I.C.E. regime.
- Return to Running Program.
- Do I Need Orthotics?
- Returning to Sport.
- Why is my injury not improving?
- Understanding Pain.
- Hip Diagnosis Guide.
Become a PhysioAdvisor Member
+ 7 References
PhysioAdvisor relies on credible scientific sources (ideally from high quality, randomised controlled trials, when available) to guide our content creation. Read about our sourcing guidelines and how we create trusted content via our editorial policy.
- Brukner et al (2012). Brukner & Khan’s clinical sports medicine (4th ed.), 516-518. Australia: McGraw Hill Education.
- Griffin DR, Dickenson EJ, O’Donnell J, Agricola R, Awan T, Beck M et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016; 50(19):1169-76.
- Chaudhry H, Ayeni OR. The etiology of femoroacetabular impingement: what we know and what we don’t. Sports Health. 2014 Mar;6(2):157-61.
- Murphy NJ, Eyles J, Bennell KL, Bohensky M, Burns A, Callaghan FM et al. Protocol for a multi-centre randomised controlled trial comparing arthroscopic hip surgery to physiotherapy-led care for femoroacetabular impingement (FAI): the Australian FASHIoN trial. BMC Musculoskelet Disord. 2017 Sep 26;18(1):406
- Casartelli NC, Maffiuletti NA, Bizzini M, Kelly BT, Naal FD, Leunig M. The management of symptomatic femoroacetabular impingement: what is the rationale for non-surgical treatment? Br J Sports Med. 2016 May;50(9):511-2.
- Mansell NS, Rhon DI, Marchant BG, Slevin JM, Meyer JL. Two-year outcomes after arthroscopic surgery compared to physical therapy for femoracetabular impingement: A protocol for a randomized clinical trial. BMC Musculoskelet Disord. 2016 Feb 4;17:60..
- Mansell NS, Rhon DI, Meyer J, Slevin JM, Marchant BG. Arthroscopic Surgery or Physical Therapy for Patients With Femoroacetabular Impingement Syndrome: A Randomized Controlled Trial With 2-Year Follow-up. Am J Sports Med. 2018 Feb 1:363546517751912. doi: 10.1177/0363546517751912.
- Murphy NJ, Eyles J, Bennell KL, Bohensky M, Burns A, Callaghan FM et al. Protocol for a multi-centre randomised controlled trial comparing arthroscopic hip surgery to physiotherapy-led care for femoroacetabular impingement (FAI): the Australian FASHIoN trial. BMC Musculoskelet Disord. 2017 Sep 26;18(1):406.
- Hip Pain and FAI – Physio Edge podcast 074 with @JoannaLKemp
- Hip pain in adults. (2016). nhs.uk/conditions/hip-pain/

Link to this Page
If you would like to link to this article on your website, simply copy the code below and add it to your page:
<a href="https://physioadvisor.com.au/injuries/hip-groin/femoroacetabular-impingement”>Femoroacetabular Impingement (FAI) – PhysioAdvisor.com</a><br/>Femoroacetabular impingement (FAI) is a condition involving increased bony growth of one or both bones that form the ball and socket joint of the hip.
Return to the top of Femoroacetabular Impingement (FAI).












