Osteitis Pubis
Updated:
(Also known as Pubic Symphysitis)
What is osteitis pubis?
Osteitis pubis is an overuse injury characterized by tissue damage and inflammation to the pelvis at the site where the two pubic bones join (pubic symphysis), resulting in groin pain.
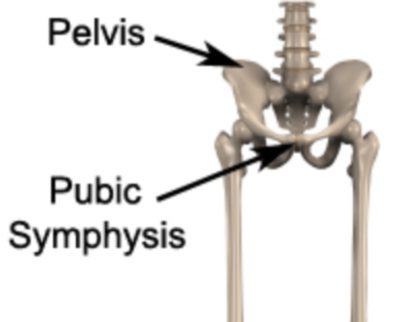
The pelvis is made up of two bones (hemipelvis). These two bones join together at the front of the pelvis at the pubic symphysis (figure 1). The pubic symphysis is made of cartilage which helps absorb forces between the two bones. There are several muscles that attach near the pubic symphysis (i.e. the adductors and abdominals). As these muscles contract (such as during running, kicking or performing sit-ups) a pulling force is exerted on the pubic symphysis. When these forces are excessive due to too much repetition or high force, damage to the pubic bones or symphysis may occur. When this results in inflammation to the pubic symphysis the condition is known as osteitis pubis.
Causes of osteitis pubis
Osteitis pubis is usually an overuse injury, which commonly occurs due to repetitive or prolonged activities placing strain on the pubic symphysis. This typically occurs due to repetitive running, kicking or change of direction activities. It is commonly seen in running sports such as football, hockey and athletics (particularly marathon runners).
Patients may also develop osteitis pubis due to excessive abdominal muscle contraction (such as during repetitive sit ups) or following inadequate rehabilitation of other injuries, such as adductor tendinopathy.
Signs and symptoms of osteitis pubis
Patients with osteitis pubis typically experience groin pain that develops gradually overtime. Pain may be experienced on one or both sides of the groin. Pain can sometimes also be experienced in the lower abdominals or at the front of the hips. Patients usually experience pain on firmly touching the pubic bone at the front of the pelvis (pubic symphysis – figure 1). Pain may also increase when squeezing the legs together or when moving the affected leg away from the midline of the body (abduction). Pain is usually aggravated by exercise such as running, kicking, performing sit-ups or change of direction activities.
In less severe cases of osteitis pubis, patients may only experience an ache or stiffness in the groin that increases upon rest following activity. These activities typically include running (particularly involving change of direction) and kicking. The pain associated with osteitis pubis may also warm up with activity in the initial stages of the condition.
As the condition progresses, patients may experience symptoms that increase during activity and affect performance. In severe cases the patient may be unable to continue the activity and may limp or ‘waddle’ as a result of the pain.
Diagnosis of osteitis pubis
A thorough subjective and objective examination from a physiotherapist is usually sufficient to diagnose osteitis pubis. Further investigations such as an X-ray, bone scan, MRI or CT scan may be required to assist with diagnosis and assess the severity of the condition.
Treatment for osteitis pubis
Most patients with osteitis pubis heal well with appropriate physiotherapy. The success rate of treatment is largely dictated by patient compliance. One of the key components is that the patient rests sufficiently from ANY activity that increases their pain until they are symptom free. In severe cases, the use of crutches when walking may be necessary to protect the pubic bones and symphysis from further damage and to hasten the healing process.
Activities which place large amounts of stress through the groin should also be minimized, these include: running (especially with change of directions), kicking, jumping and sit-ups. By avoiding these activities, the body can begin the healing process in the absence of further tissue damage. Once the patient can perform these activities pain-free a gradual return to these activities is indicated provided there is no increase in groin symptoms. Activities which do not cause pain or an increase in symptoms are usually encouraged during the rehabilitation period to maintain fitness.
Ignoring symptoms or adopting a ‘no pain, no gain’ attitude is likely to lead to the condition becoming chronic and requiring an extensive period of rehabilitation. Immediate, appropriate treatment in patients with osteitis pubis is therefore essential to ensure a speedy recovery. Once the condition is chronic, healing slows significantly resulting in markedly increased recovery times and an increased likelihood of future recurrence.
Ice therapy and anti-inflammatory medication can significantly reduce the inflammation and pain associated with osteitis pubis. Simply resting and taking anti-inflammatories alone however, will not completely resolve the condition unless it is accompanied by appropriate physiotherapy treatment.
A graduated flexibility, core stability and strengthening program guided by a physiotherapist is essential to rehabilitate the injured patient and reduce the likelihood of recurrence. Careful assessment by the physiotherapist to determine which factors have contributed to the development of osteitis pubis, with subsequent correction of these factors is essential to ensure an optimal outcome. Without this, symptoms are most likely to recur upon resumption of the aggravating activity.
A graduated return to activity program in the final stages of rehabilitation is essential for a safe and successful return to sport or activity. For those who wish to return to sport, this should include a return to running program, the implementation of progressive acceleration and deceleration running drills, as well as change of direction drills before returning to match play. These progressions should be carefully monitored by the treating physiotherapist for any aggravation of symptoms.
Prognosis of osteitis pubis
Osteitis pubis can often be a difficult injury to rehabilitate. However, with appropriate physiotherapy and management, most patients can return to normal function in a number of weeks. In more severe cases (particularly in those patients who have had their symptoms for a long period of time) rehabilitation may take significantly longer, often lasting 6 months or more before a successful return to sport can occur. Early physiotherapy treatment is therefore vital to hasten recovery in all patients with this condition.
Contributing factors to the development of osteitis pubis
There are several factors which can predispose patients to developing osteitis pubis. These need to be assessed and corrected with direction from a physiotherapist. Some of these factors include:
- poor biomechanics
- muscle weakness (especially of the adductors, gluteals or core stabilisers)
- inadequate rehabilitation following a previous adductor injury
- muscle tightness (particularly of the adductors, gluteals, hip flexors, hamstrings, or abdominals)
- inappropriate training or technique
- a change in training conditions or surfaces
- a recent increase in training frequency or intensity
- poor posture
- poor foot posture (e.g. flat feet)
- inappropriate footwear
- decreased fitness
- fatigue
- inadequate warm up
- joint stiffness (particularly the lower back, hip and knee)
- poor pelvic and core stability
- neural tightness
- muscle imbalances
Physiotherapy for osteitis pubis
Physiotherapy for patients with osteitis pubis is vital to hasten the healing process, ensure an optimal outcome and reduce the likelihood of future recurrence. Treatment may comprise:
- soft tissue massage (particularly to the adductors, abductors, abdominals and psoas muscles)
- electrotherapy (e.g. ultrasound)
- stretches
- muscle energy techniques
- joint mobilization (in particular the lumbar spine and hip joint)
- ice or heat treatment
- education
- biomechanical correction
- the use of crutches
- dry needling
- neural stretches
- progressive exercises to improve strength, flexibility, core stability, pelvic stability and balance
- clinical Pilates
- hydrotherapy
- activity modification advice
- technique correction
- anti-inflammatory advice
- prescription of orthotics or footwear advice
- devising and monitoring a return to sport or activity plan
Other intervention for osteitis pubis
Despite appropriate physiotherapy management, some patients with osteitis pubis do not improve adequately. When this occurs, the treating physiotherapist or doctor can advise on the best course of management. This may include investigations such as an X-ray, ultrasound, CT scan or MRI, pharmaceutical intervention, corticosteroid injection or referral to appropriate medical authorities who can advise on any intervention that may be appropriate to improve the condition. A review with a podiatrist may be indicated for the prescription of orthotics in patients with abnormal foot biomechanics. In very rare cases, surgical intervention may be considered.
Exercises for osteitis pubis
The following exercises are commonly prescribed to patients with osteitis pubis. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 3 times daily and only provided they do not cause or increase symptoms.
Transversus Abdominus Retraining
Begin this exercise in lying or standing (figure 2). Slowly pull your belly button in “away from your belt line” and breathe normally. Your rib cage should remain relaxed and should not elevate during this process. You should be able to feel the muscle contracting if you press deeply 2cm in from the bony process at the front of your pelvis. Practise holding this muscle at one third of a maximal contraction for as long as possible during everyday activity (e.g. when walking etc.) provided it does not increase your symptoms. Repeat 3 times daily

Adductor Stretch
Begin this exercise by standing tall with your back straight and your feet approximately twice shoulder width apart. Gently lunge to one side, keeping the other knee straight, until you feel a stretch in the groin or as far as you can go without pain (figure 3). Ensure the stretch is pain-free. Hold for 15 seconds and repeat 4 times at a mild to moderate stretch provided there is no increase in symptoms.

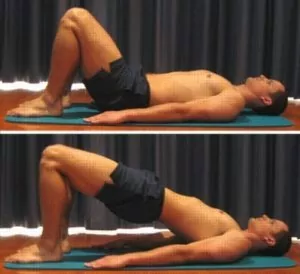
Bridging
Begin this exercise lying on your back in the position demonstrated (figure 4). Slowly lift your bottom pushing through your feet, until your knee, hip and shoulder are in a straight line. Tighten your bottom muscles (gluteals) as you do this. Hold for 2 seconds and repeat 10 times provided the exercise is pain free.
Find a Physio for osteitis pubis
Find a physiotherapist in your local area who can treat osteitis pubis.
Physiotherapy products for osteitis pubis
Some of the most commonly recommended products by physiotherapists to hasten healing and speed recovery in patients with osteitis pubis include:
To purchase physiotherapy products for osteitis pubis click on one of the above links or visit the PhysioAdvisor Shop.
Other Exercises
- View more Hip Flexibility Exercises.
- View more Hip Strengthening Exercises.
- View Basic Pilates Exercises to improve core stability and posture.

Link to this Page
If you would like to link to this article on your website, simply copy the code below and add it to your page:
<a href="https://physioadvisor.com.au/injuries/hip-groin/osteitis-pubis”>Osteitis Pubis – PhysioAdvisor.com</a><br/>PhysioAdvisor offers detailed physiotherapy information on osteitis pubis including: diagnosis, treatment, exercises, physiotherapy products and more...
Return to the top of Osteitis Pubis.



