Spondylolysis
Updated:
(Also known as Pars Defect, Lumbar Stress Fracture, Lumbar Spine Stress Fracture, Stress Fracture of the Pars Interarticularis)
What is a spondylolysis?
A spondylolysis is the name given to a stress fracture of the lumbar spine (lower back) and specifically affects a region of bone known as the pars interarticularis (figure 1).
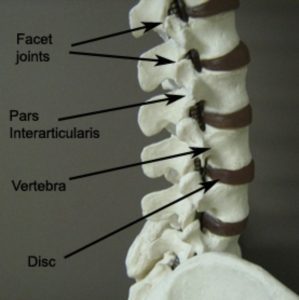
The spine comprises of many bones known as vertebrae. Each vertebra connects with the vertebra above and below via two types of joints: the facet joints on either side of the spine and the disc centrally (figure 1). These joints are designed to support body weight and enable spinal movement.
During certain movements of the spine, compressive force is placed on the facet joint. This force is then transmitted through a bony region known as the ‘pars interarticularis’ (figure 1). If these forces are excessive and beyond what the bone can withstand, bony damage will occur. This initially results in a bony stress reaction, however, with continued damage may progress to a bony stress fracture of the pars interarticularis. This condition is known as a spondylolysis.
A spondylolysis typically occurs on one side of the spine, however, occasionally both sides may be involved. This can result in one vertebra slipping forwards on another and is known as a spondylolisthesis.
Causes of a spondylolysis
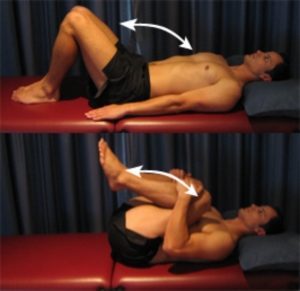
A spondylolysis usually occurs as a result of repetitive or forceful hyperextension activities (i.e. excessive backward bending of the spine – figure 2), especially when they are combined with rotation. They are typically overuse injuries and are more common in the younger athlete whose bones are yet to reach skeletal maturity.

A spondylolysis is most commonly seen in the following sports:
- cricket (fast bowling)
- gymnastics
- tennis
- dance
- weight lifting
- wrestling
- pole vaulting
- high jump
- throwing sports (javelin, baseball pitching etc.)
Signs and symptoms of a spondylolysis
Patients with this condition typically experience pain on one side of the lower back that progressively increases with movements involving hyperextension (figure 2). Symptoms generally decrease with rest. Pain in the lower back is usually felt on the opposite side of the body to the arm performing the repetitive movement (e.g. left sided back pain for a right arm bowler etc). Pain can usually be reproduced by firmly pressing on the affected area, or, by extending backwards whilst standing on the affected leg, with the aid of a therapist.
Diagnosis of a spondylolysis
A thorough subjective and objective examination from a physiotherapist may be sufficient to diagnose a spondylolysis. X-rays may or may not demonstrate a stress fracture, depending on the severity of injury. Usually a bone scan is used to confirm an area of bony damage. Following this, a CT scan may be used to determine the presence of a stress fracture. Occasionally, other investigations such as an MRI may be indicated.
Treatment for a spondylolysis

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Prognosis of a spondylolysis
Rehabilitation following a spondylolysis usually occurs over weeks to months with direction from a physiotherapist and will vary depending on the severity of injury. With appropriate treatment, most minor stress fractures should be able to achieve bony union in 6 to12 weeks. Once this is achieved and the patient is symptom free, a gradual and progressive return to activity is indicated under guidance from a physiotherapist. This usually occurs over a subsequent period of approximately 4 to 6 weeks. More severe fractures may require an extended period of rehabilitation of approximately 6 to 12 months.
In some cases, a stress fracture may result in non-union of the bone and ongoing problems (especially if they are managed inappropriately). Accurate diagnosis, treatment and management in the early stage is therefore vital.
Physiotherapy for a spondylolysis
Physiotherapy for patients with this condition can hasten the healing process, reduce the likelihood of future recurrence and ensure a safe return to activity. Treatment may comprise:
- soft tissue massage
- electrotherapy (e.g. ultrasound)
- joint mobilization
- trigger point therapy
- dry needling
- education
- activity modification advice
- the use of a back brace
- biomechanical correction
- sporting technique correction
- clinical Pilates
- hydrotherapy
- exercises to improve flexibility, strength, posture and core stability
- a graduated return to activity program
Contributing factors to the development of a spondylolysis
There are several factors that may contribute to the development of this condition. These need to be assessed and corrected with direction from a physiotherapist and may include:
- poor sporting technique
- inappropriate or excessive training or activity
- inadequate recovery periods from training or activity
- joint stiffness (particularly the lumbar or thoracic spine or hips)
- muscle weakness (particularly the core stabilisers and gluteals)
- muscle tightness (particularly the hip flexors, gluteals or hamstrings)
- poor posture
- poor foot biomechanics
- age (particularly adolescence)
- anatomical anomalies
- inappropriate sporting surfaces
Other intervention for a spondylolysis
Despite appropriate physiotherapy management, a small percentage of patients with this condition fail to improve adequately and may require other intervention. This may include pharmaceutical intervention, corticosteroid injection, further investigations such as X-rays, CT scan, MRI or bone scan or assessment from an orthopaedic specialist who can advise on any procedures that may be appropriate for the condition. The treating physiotherapist can advise if this is required and will refer to the appropriate medical authority if it is warranted clinically.
Exercises for a spondylolysis
The following exercises are commonly prescribed to patients with this condition. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 3 times daily and only provided they do not cause or increase symptoms.
Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate, advanced and other exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms.
Initial Exercises
Transversus Abdominus Retraining
Slowly pull your belly button in “away from your belt line” and breathe normally. Your rib cage should remain relaxed and should not elevate during this process. You should be able to feel the muscle contracting if you press deeply 2cm in from the bony process at the front of your pelvis (figure 3). Practise holding this muscle at one third of a maximal contraction for as long as possible during everyday activity (e.g. when walking etc.) provided it is pain free. Repeat 3 times daily.

Rotation in Lying
Begin this exercise lying on your back as demonstrated (figure 4). Slowly take your knees from side to side as far as you can go without pain and provided you feel either nothing, or, no more than a mild to moderate stretch. Repeat 10 times to each side provided the exercise is pain free.

Knees to Chest
Begin lying on your back with your knees bent. Slowly take both knees towards your chest using your hands to assist as far as you can go without pain and provided you feel either nothing, or, no more than a mild to moderate stretch (figure 5). Repeat 5 – 10 times provided the exercise is pain free.
Intermediate Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Advanced Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Other Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Rehabilitation Protocol for a spondylolysis

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Physiotherapy products for a spondylolysis
Some of the most commonly recommended products by physiotherapists to hasten healing and speed recovery in patients with this condition include:
-
 Wheat Bags
Wheat Bags -
 Oppo Industrial Back Support (OPP2169)
Oppo Industrial Back Support (OPP2169) -
 AllCare Ortho Light Back Support
AllCare Ortho Light Back Support -
 Premium Strapping Tape 38mm (Victor)
Premium Strapping Tape 38mm (Victor) -
 AllCare Pro-TENS Machine
AllCare Pro-TENS Machine -
 AllCare Spikey Massage Ball
AllCare Spikey Massage Ball -
 Fixomull Stretch 5cm x 10m
Fixomull Stretch 5cm x 10m -
 AllCare Instant Cold Pack (15 x 25cm)
AllCare Instant Cold Pack (15 x 25cm) -
 AllCare Foam Roller Round
AllCare Foam Roller Round -
 66fit Water Running Belt
66fit Water Running Belt -
 McKenzie Treat Your Own Back Book
McKenzie Treat Your Own Back Book -
 Lumbar Rolls (‘D’ Shaped)
Lumbar Rolls (‘D’ Shaped)
To purchase physiotherapy products for a spondylolysis, click on one of the above links or visit the PhysioAdvisor Shop
Find a Physio for a spondylolysis
 Find a physiotherapist in your local area who can treat this condition.
Find a physiotherapist in your local area who can treat this condition.
Other Exercises
- View more Lower Back Stretches.
- View more Lower Back Strengthening Exercises.
- View more Core Exercises.
- View Basic Pilates Exercises.
More Information
- View detailed information on when to use Ice or Heat .
- View detailed information on initial injury management and the R.I.C.E. Regime.
- View detailed information on Warming Up and Cooling Down.
- View detailed information on Return to Running Program.
- View detailed information on Returning to Sport.
- View our Lower Back Diagnosis Guide
Become a PhysioAdvisor Member

Link to this Page
If you would like to link to this article on your website, simply copy the code below and add it to your page:
<a href="https://physioadvisor.com.au/injuries/lower-back/spondylolysis”>Spondylolysis – PhysioAdvisor.com</a><br/>A spondylolysis is the name given to a stress fracture of the lumbar spine (lower back) and specifically affects a region of bone known as the pars interarticularis.
Return to the top of Spondylolysis.


