Hip Replacement
Updated:
(Also known as Total Hip Replacement, Total Hip Joint Replacement, Hip Replacement Surgery, Total Hip Arthroplasty)
What is a hip replacement?
A hip replacement is an invasive surgical procedure that is used to remove a diseased hip joint (most commonly due to osteoarthritis) and replace it with an artificial joint or prosthesis.
The hip joint is a ball and socket joint that comprises of the union of the long bone of the thigh forming the ball (femur) and the acetabulum (pelvis) forming the socket (figure 1). Articular cartilage lines the joint surfaces acting as a shock absorber and cushioning the impact of the femur on the pelvis during weight-bearing activity. In addition, strong ligaments and connective tissue hold the bones of the hip together, giving it stability.
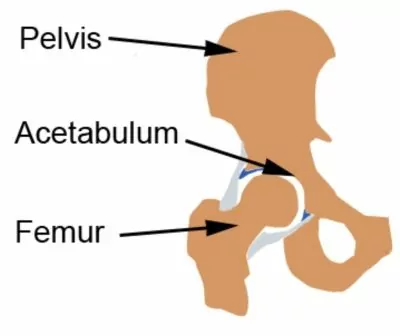
Figure 1 – Hip Replacement Anatomy
Structures within the hip (such as the cartilage or bony joint surfaces) may be damaged due to overuse, trauma or certain conditions (e.g. rheumatoid arthritis, tumours etc.). This may lead to degenerative changes within the hip or osteoarthritis. These injuries may be beyond the body’s healing capacity and if severe enough may warrant hip replacement surgery to treat the condition. This may be particularly indicated in patients with severe hip osteoarthritis who have not responded to appropriate physiotherapy treatment and rehabilitation, and, have severe pain and disability due to their hip condition.
A hip replacement is usually performed under general anesthetic and usually takes approximately 2-4 hours. Medications, such as antibiotics, are usually administered prior to surgery to prevent potential complications such as infection.
Hip replacement surgery usually involves an incision of approximately 20 – 30cm that is made over the top of the hip. Soft tissue, such as muscle, is moved to expose the hip joint, followed by cutting and removal of the damaged joint surfaces of the acetabulum and femur. The prosthesis is then fixated into position with the use of bone cement to hold the prosthesis in place or alternatively a prosthesis without cement may be used with microscopic pores enabling normal bony growth from the femur into the prosthesis. Plastic or metal are typically used to replace the socket of the hip with metal or ceramic used to replace the stem. A drainage tube is placed into the wound and a urinary catheter is sometimes inserted. The wound is closed with stitches or clips. Hip replacement surgery without complications usually involves a 3 – 5 day hospital stay (although this varies from patient to patient depending on post operative progress).
Indications for a hip replacement
Hip replacement surgery may be indicated in patients with certain hip conditions, particularly those that do not respond to appropriate physiotherapy treatment and rehabilitation, and, have severe pain and disability.
Some of the more common hip conditions treated with a hip replacement include:
- Severe osteoarthritis
- Rheumatoid arthritis
- Ligament damage or infection that leads to severe osteoarthritis
- Gout
- Avascular necrosis (death of bone following loss of blood supply)
- Some hip fractures (particularly those with a high likelihood of avascular necrosis).
- Bone dysplasias (abnormal growth of bone)
- Certain tumours
An orthopaedic surgeon can assess a patient and determine the suitability of a hip replacement based on a number of factors. Some of these may include:
- Injury diagnosis and severity
- Degree of pain and disability experienced by the patient
- Patient age, occupation and activity levels
- Expected symptomatic and functional improvement following surgery
- Medical history of the patient
- Potential complications of surgery
- Cost
Signs and symptoms following a hip replacement
Following hip replacement surgery, symptoms vary significantly from patient to patient depending on a number of factors such as the severity of injury prior to surgery, degree of trauma to tissue during surgery, type of pain relief or anti inflammatory medication used, strength and flexibility of the hip prior to surgery, age of the patient and quality of rehabilitation following the procedure.
A small percentage of patients may experience only minor symptoms following a hip replacement and may only notice stiffness and minor soreness. This is usually the case in younger patients who have had excellent strength and flexibility of the hip prior to surgery, have appropriate medication and are adhering to appropriate rehabilitation under physiotherapy guidance.
Patients usually experience swelling, pain and hip stiffness with symptoms ranging from mild to severe. Pain may be felt in the front, back or side of the hip, the groin, thigh, or occasionally the knee, calf, ankle or foot. Symptoms typically increase with excessive weight bearing activity (especially walking up hills or on uneven surfaces), with prolonged standing or sitting, with excessive bending, straightening, side elevation or twisting of the hip, when climbing stairs, or when squatting. Patients may also experience difficulty getting in and out of a vehicle or bed. The patient may also walk with a limp or be unable to weight bear due to pain. Symptoms may also increase with rest and may present as an ache, pain or stiffness that is particularly prominent at night or first thing in the morning.
Tenderness is usually experienced when firmly touching the hip region and surgical scars. An increase in local tissue temperature is also common. The hip may feel weak or unstable and in some cases may give way or feel like it’s going to collapse with certain movements. Bruising, pins and needles or numbness may also be experienced which will vary in severity from patient to patient.
Treatment following a hip replacement
Directly following hip replacement surgery the hip is usually covered with a dressing and a drainage tube is used to remove excess fluid from the wound. A pillow is usually placed between the legs to keep the hip in place. Antibiotics and blood thinning medications are usually given to reduce the risk of infection and blood clot formation. Strong pain relief is administered often via a patient controlled analgesia (PCA) pump allowing the patient to administer their own dose of pain relief on demand. A urinary catheter is sometimes inserted.
Early breathing and coughing exercises and exercises to move the feet and other leg are encouraged as soon as possible, along with the use of compressive TED stockings, to reduce the risk of clot formation and lung complications following a hip replacement. A special bed may be used to prevent the hip from bending beyond 90 degrees. An abduction pillow may also be used to keep the legs shoulder width apart and to prevent rotation of the hips.
Gentle exercises are usually prescribed by the physiotherapist to encourage healing, mobility and strength. It is common for patients to begin physiotherapy exercises Day 1 after surgery. This progresses to standing, walking and climbing stairs with the use of walking frames or crutches as guided by the treating physiotherapist and surgeon. Stitches may be dissolvable or are usually removed approximately 10 days after surgery.
Patients who have had a hip replacement are instructed to avoid crossing the leg beyond the midline of the body (e.g. not crossing the leg over the other leg), bending the hip beyond 90 degrees and twisting the hip and leg excessively as these movements may alone or in combination, dislocate the hip.
Following hip replacement surgery and discharge from hospital, most patients heal well with appropriate physiotherapy. The success rate of treatment is largely dictated by patient compliance. Crutches are usually required for days to weeks as guided by the surgeon and treating physiotherapist. Patients are usually instructed to sleep with a pillow between their legs. Activities which place large amounts of stress through the hip should be avoided particularly those which involve crossing the legs, bending the hip beyond 90 degrees, excessive twisting and weight bearing activities (such as prolonged standing or walking, lifting, squatting, jumping, running etc). Avoiding aggravating activities allows the healing process to take place in the absence of further damage.
Following a hip replacement, patients usually benefit from following the R.I.C.E. Regime. The R.I.C.E regime is beneficial in the first 72 hours following surgery or when inflammatory signs are present (i.e. morning pain, pain with rest, or new swelling). For a hip replacement, this primarily involves resting from aggravating activities, and regular icing. Anti-inflammatory medication may also significantly hasten the healing process by reducing the pain and swelling associated with inflammation.
Patients who have undergone a hip replacement should perform regular flexibility and strengthening exercises as part of their rehabilitation to ensure an optimal outcome. Emphasis is placed on restoring hip range of movement and gluteal strength. Quadriceps, hamstring and calf strengthening exercises are also important to improve the control of the hip joint with weight-bearing activities. Hydrotherapy exercises are often indicated to improve movement and strengthen the hip in a low weight bearing environment. The treating physiotherapist can advise which exercises are most appropriate for the patient and when they should be commenced.
Manual “Hands-on” Therapy from the treating physiotherapist such as massage, joint mobilization, dry needling and electrotherapy are important to improve scar tissue flexibility and range of movement. This is particularly important in the first 6 – 12 weeks following a hip replacement.
Review with an occupational therapist may be indicated to teach strategies to improve function and mobility around the home this may include the use of appropriate aids, high chairs, rails etc.
In the final stages of rehabilitation for patients with a hip replacement, a gradual return to activity can occur as guided by the treating physiotherapist provided there is no increase in symptoms.
Prognosis following a hip replacement
The vast majority of patients who undergo this procedure experience less pain and improved mobility compared to preoperatively. Recovery times vary significantly from patient to patient although rehabilitation typically lasts 3 – 12 months or longer. It is important to note that a hip replacement will not function the same as a normal hip.
In patients with more severe hip injuries with subsequent severe weakness or hip stiffness prior to hip replacement surgery, or in those who experience other surgical complications, such as infection, or damage to local blood vessels or nerves, rehabilitation may require an extended period. Following surgery, patients who do not rest adequately from aggravating activities (e.g. excessive walking, standing, bending of the hip past 90 degrees, crossing of the legs or twisting) or those who do not perform exercises appropriately may also prolong their recovery.
In well selected patients for a hip replacement, the prosthesis lasts greater than 15 years in approximately 95% of patients although excessive wear and tear may reduce prosthesis longevity. It is particularly important to maintain a healthy weight as obesity may reduce the life span of a hip replacement.
Physiotherapy following a hip replacement
Physiotherapy treatment is vital to hasten the healing process and ensure an optimal outcome in all patients following a hip replacement. This should ideally begin prior to surgery. Treatment may comprise:
- soft tissue massage
- electrotherapy
- the use of crutches or other walking aids
- joint mobilization
- dry needling
- hydrotherapy
- ice or heat treatment
- progressive exercises to improve flexibility, strength (especially the gluteal and quadriceps muscles), balance and core stability
- activity modification advice
- education
- biomechanical correction
- anti-inflammatory advice
- weight loss advice where appropriate
- a gradual return to activity program
Potential complications following a hip replacement
Some of the potential complications of hip replacement surgery may include:
- Wound Infection
- Allergic reaction to the anesthetic
- Joint dislocation
- Scarring and limitation of movement of the hip
- Failure of the prosthesis (breaking or loosening)
- Fracture of the bone during or after surgery
- Difficulty with urination
- Damage to blood vessels in the leg
- Temporary or permanent numbness around the incision
- Paralysis of the leg due to nerve damage
- Lung infection
- Deep vein thrombosis
- Pulmonary Embolism
- Heart Attack
- Stroke
- Death
Other intervention following a hip replacement
Despite appropriate physiotherapy management, some patients fail to improve adequately following hip replacement surgery. When this occurs the treating physiotherapist, doctor or orthopedic surgeon can advise on the best course of management. This may include further investigations, pharmaceutical intervention, or further surgery.
Exercises following a hip replacement
The following exercises are commonly prescribed to patients following a hip replacement. These can usually commence once the orthopaedic surgeon or physiotherapist have indicated it is safe to do so. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 3 – 4 times daily and only provided they do not cause or increase symptoms.
Knee Towards Chest
Gently bring your knee towards your chest as far as possible and comfortable and not beyond a 90 degree angle, without increasing your pain (figure 2). Aim for no more than a mild to moderate stretch. Repeat 10 – 20 times provided there is no increase in symptoms.

Hip Abduction
Begin this exercise lying on your back (figure 3). Keeping your knee straight, take your leg to the side as far as possible and comfortable without increasing your pain, then return to the starting position (do not cross your leg past the mid line of the body). Keep your knee cap and toes facing the ceiling throughout the exercise. Repeat 10 – 20 times provided there is no increase in symptoms.

Hip External Rotation
Begin this exercise lying on your back with your knee bent and foot flat on the floor. Take your knee to the side as far as possible and comfortable without increasing pain, then return to the starting position (do not let your knee or leg cross the midline of the body). Repeat 10 – 20 times provided there is no increase in symptoms.

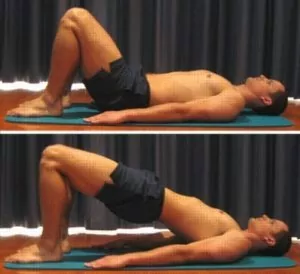
Bridging
Begin this exercise by lying on your back in the position demonstrated (figure 5). Slowly lift your backside, pushing through your feet, until your knees, hips and shoulders are in a straight line. Tighten your backside muscles (gluteals) as you do this and hold for 2 seconds. Then slowly return to the starting position. Repeat 10 times provided there is no increase in symptoms.
Quads Over Fulcrum
Begin this exercise lying on your back with a rolled towel or Foam Roller under your knee and your knee relaxed (figure 6). Slowly straighten your knee as far as possible tightening the front of your thigh (quadriceps). Hold for 5 seconds and repeat 10 times as hard as possible without increasing your symptoms.

Physiotherapy products following a hip replacement
Some of the most commonly recommended products by physiotherapists to hasten healing and speed recovery in patients who have had a hip replacement include:
To purchase physiotherapy products following a hip replacement click on one of the above links or visit the PhysioAdvisor Shop.
More Information
- View more Hip Flexibility Exercises
- View more Hip Strengthening Exercises.
- Read about How to use Crutches
Find a Physio following a hip replacement
Find a physiotherapist in your local area who can treat patients prior to, or following, a hip replacement.

Link to this Page
If you would like to link to this article on your website, simply copy the code below and add it to your page:
<a href="https://physioadvisor.com.au/injuries/hip-groin/hip-replacement”>Hip Replacement – PhysioAdvisor.com</a><br/>PhysioAdvisor offers detailed physiotherapy information on a hip replacement including: indications, signs and symptoms, treatment, prognosis, exercises, physiotherapy products and more...
Return to the top of Hip Replacement.



