Spinal Degeneration
Updated:
(Also known as Degenerative Spine, Back Arthritis, Osteoarthritis of the Spine, Spinal Arthritis, Disc Degeneration, Spinal Canal Stenosis, Vertebral Canal Stenosis, Spinal Stenosis)
What is spinal degeneration?
Spinal degeneration is a condition characterised by gradual wear and tear to the discs, facet joints and bones of the spine that typically occurs in older patients.
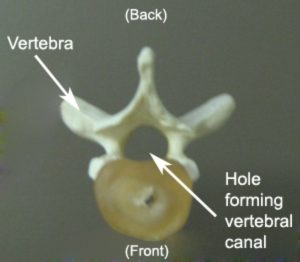
The spine consists of numerous bones (vertebrae) situated on top of each other. Each individual vertebra comprises of several bony projections and a large hole within its centre (figure 1). The hole within these vertebrae line up with adjacent vertebrae, forming the spinal canal. The spinal canal houses the spinal cord and nerves, providing space and protection for these structures to travel between the brain and body.
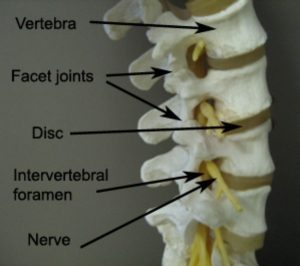
The spinal vertebrae connect with each other via the intervertebral disc (located centrally) and the facet joints (located on each side of the spine) (figure 2). Small holes are also situated between adjacent vertebrae on each side of the spine. These holes are known as intervertebral foramen and provide an exit point for nerves to leave the spinal canal (figure 2).
Degeneration of the spine may occur due to gradual wear and tear to the bones and intervertebral joints (i.e. facet joints and discs) over time. The anatomical changes associated with this process may include:
- Reduced disc height
- Joint cartilage loss
- Osteophyte formation (i.e. Bony spurring)
- Roughening of joint surfaces
- Bone thickening
When some or all of these changes occur, the condition is known as spinal degeneration. With further progression over time, the intervertebral foramen and spinal canal may also start to narrow. This can lead to spinal canal stenosis (i.e. narrowing of the canal) or foraminal stenosis (i.e. narrowing of the intervertebral foramen) and when severe enough may result in compression of the spinal cord or nerves.
Spinal degeneration typically occurs in older patients but may commence as early as the second decade of life. It is more likely to affect lower vertebral levels (i.e. L3 – S1) perhaps due to increased mechanical stress associated with greater weight bearing forces on these levels.
Causes of spinal degeneration
Spinal degeneration usually occurs gradually over a prolonged period of time. This typically occurs in association with gradual wear and tear due to overuse, or, as part of the aging process. Spinal degeneration may be more common in patients with a past history of lower back pain or spinal trauma. Patients who are overweight, smoke, have a family history of degeneration, or, have a lifestyle comprising excessive bending, lifting, twisting or sitting may also be more likely to develop the condition.
Symptoms of spinal degeneration
Minor cases of spinal degeneration often cause little or no symptoms for patients. This may also be the case for some patients with moderate degeneration and a smaller percentage of patients with severe degeneration. As the condition deteriorates and becomes symptomatic, patients may experience lower back, buttock or hip pain, loss of spinal movement, muscle spasm and general lower back stiffness. In severe cases entailing compression of the spinal cord or nerves, intense pain, parasthesia (i.e. pins and needles or numbness) or weakness may be experienced in the lower back, buttocks, thigh, groin, lower legs or feet. In some cases patients may be noticeably out of alignment, or, may walk with a limp.
Patients who experience pain due to this condition generally experience increased symptoms during activities that forcefully, continuously or repetitively straighten or extend the spine (figure 3). Activities that place weight on the spine (e.g. lifting, prolonged standing, walking etc.) may also exacerbate symptoms. Relief from symptoms may occur during activities that bend the spine (e.g. sitting) or take weight off it (i.e. lying down). Symptoms may also ease with warmer weather or when applying warmth to the lower back (e.g. a hot pack, hot shower or bath).

Diagnosis of spinal degeneration
A comprehensive examination by a physiotherapist is usually sufficient to form a clinical diagnosis of spinal degeneration. Radiological investigation (typically in the form of X-Rays) is required to confirm diagnosis. Occasionally, MRI, CT scan or bone scan may be indicated to further evaluate the severity of the condition and determine the involvement of other structures.
It is important to note, that radiological findings of degeneration alone, do not automatically mean that symptoms are arising from these structures. Correlation with clinical examination is essential to determine the likely origin of symptoms.
Treatment for spinal degeneration

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Prognosis of spinal degeneration
Although the degenerative changes associated with this condition are largely irreversible, most patients can expect a good prognosis with appropriate physiotherapy management. The majority of patients with mild to moderate spinal degeneration who are managed appropriately can often experience minimal or no symptoms. These patients can also generally remain active with some recreational or lifestyle modifications. Patients who have severe degenerative changes can also improve significantly with appropriate management. However, these patients often require more prominent lifestyle modification and typically experience more significant functional limitation and symptoms.
Physiotherapy for spinal degeneration
Physiotherapy treatment is important to minimise symptoms and improve strength, flexibility and activity tolerance in patients with spinal degeneration. Appropriate treatment can optimise the long term outcome and may entail:
- education
- activity modification advice
- exercises to improve flexibility, strength, core stability and functional tolerance
- clinical Pilates
- hydrotherapy
- postural correction
- the use of a back brace or back taping
- prescription of walking aids
- soft tissue massage
- joint mobilisation
- electrotherapy (such as ultrasound)
- traction
- dry needling
- ice or heat treatment
- the use of a lumbar support for sitting
- weight loss or smoking cessation advice (where appropriate)
Factors contributing to the development of spinal degeneration
There are numerous factors which may in isolation or combination contribute to the development of this condition. These factors should be assessed and corrected, where possible, by an experienced physiotherapist. These contributing factors may include:
- increasing age (particularly > 40 years)
- being overweight or obese
- smoking
- genetics / family history
- a lifestyle involving excessive lifting, sitting, bending or twisting
- a history of lower back trauma or injury
- excessive or inappropriate training or activity
- insufficient recovery periods from training or activity
- inadequate lower back flexibility
- poor posture or core stability
- inappropriate lifting technique
- muscle weakness, tightness or imbalances
- biomechanical abnormalities
Other intervention for spinal degeneration
Some patients with spinal degeneration do not improve adequately, despite having appropriate physiotherapy treatment and management. In these situations, other intervention may be indicated. This may include:
- pharmaceutical review (for appropriate medication)
- the use of natural supplements (such as fish oil, tumeric, glucosamine and chondroitin)
- cortisone injection
- further investigation (e.g. X-rays, MRI, CT scan or bone scan)
- referral to a specialist or sports doctor.
- referral to other health professionals (such as a pain psychologist, dietician etc.)
Your treating physiotherapist can provide advice on the most appropriate course of action in your situation and refer you to other medical professionals as indicated. In patients with severe spinal degeneration involving spinal cord or nerve root compression (typically due to spinal canal stenosis), surgery may be indicated to reduce compression of neural structures.
Exercises for spinal degeneration
The following exercises are frequently prescribed to patients with spinal degeneration in clinical practise. The suitability of these exercises should be discussed with your treating physiotherapist prior to commencement. Generally, the exercises should be performed 3 times daily and only provided they do not cause or increase symptoms.
Your physiotherapist can advise when to begin the initial exercises and progress to the intermediate, advanced and other exercises. As a general rule, the addition or progression of exercises should take place provided there is no symptomatic increase.
Initial Exercises
Transversus Abdominus (TA) Activation
Begin this exercise lying in optimal posture (with or without a pillow for comfort). Gently pull your belly / navel in “away from your belt line” ensuring you breathe normally. Keep your rib cage relaxed and ensure there is no chest elevation when doing this. To ensure activation, feel your transversus abdominus muscle contract by placing your fingers deeply into your abdomen, a few cm in from the bony prominence located at the front of your pelvis (on each side – figure 4). Try to maintain activation of this muscle at 1/3 of a maximal contraction and for as long as possible during daily activity (for example whilst walking). Repeat this exercise 3 times per day provided there is no increase in symptoms.

Spinal Rotation in Lying
Start this exercise in the position demonstrated (figure 5). Gently move your knees from one side to the other as far as you can go without discomfort and provided you feel no greater than a mild to moderate stretching sensation. Repeat this exercise 10 times provided there is no increase in symptoms.

Hip Flexion
Slowly take your knee towards your chest as far as you can go without pain and provided you feel no more than a mild to moderate stretch (figure 6). Use your hands to gently bring your knee closer to your chest. Repeat 5 – 10 times on each leg provided there is no increase in symptoms.

Intermediate Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Advanced Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Other Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Rehabilitation Protocol for spinal degeneration

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Physiotherapy products for spinal degeneration
Some of the most commonly recommended products by physiotherapists to help patients with this condition include:
To purchase physiotherapy products to assist with degeneration of the spine, click on one of the above links or visit the PhysioAdvisor Shop.
 More Exercises
More Exercises
- Lower Back Stretches.
- Lower Back Strengthening Exercises.
- Basic Pilates Exercises.
- Cardiovascular Exercise.
- Core Stability Exercises.
 Recommended Reading
Recommended Reading
- Ice or Heat
- Initial injury management and the R.I.C.E. Regime
- Safe Lifting
- Correct Posture
- Ergonomic Computer Setup
- Back Taping Techniques
- Understanding Pain
- Why Is My Injury Not Improving?
- Lower Back Pain Diagnosis Guide
 Find a Physio for spinal degeneration
Find a Physio for spinal degeneration
Find a physiotherapist in your local area who can assess and treat degeneration of the spine.
Become a PhysioAdvisor Member

Link to this Page
If you would like to link to this article on your website, simply copy the code below and add it to your page:
<a href="https://physioadvisor.com.au/injuries/lower-back/spinal-degeneration”>Spinal Degeneration – PhysioAdvisor.com</a><br/>PhysioAdvisor offers detailed physiotherapy information on spinal degeneration and back arthritis including signs and symptoms, diagnosis, treatment, exercises, physiotherapy products and more...
Return to the top of Spinal Degeneration.