Pelvic Floor Dysfunction
Updated:
What is pelvic floor dysfunction
Pelvic floor dysfunction is a condition characterised by a range of potential symptoms and issues which may occur in association with excessive stretching, weakness or tightness of the pelvic floor muscles. Symptoms may include:
- pelvic pain
- urinary or faecal incontinence
- incomplete emptying
- prolapse i.e. sagging of internal organs – where the uterus, bladder or bowel fall out of position
- suboptimal sexual health
The pelvic floor muscles sit deeply at the base of the abdomen, forming a sling between the coccyx (tail bone) at the back and the pubic bone at the front. They are primarily responsible for supporting the bowel, bladder (and uterus, in women) and controlling bowel and bladder function (such as allowing you to ‘hold on’ until an appropriate time and place). They also act to stabilise the pelvis (therefore impacting lower back stability) and are an important component of optimal sexual health.
There are many factors which may act in isolation or combination to cause impairment of these muscles and subsequent pelvic floor dysfunction. Some of the more common factors may include:
- Being pregnant and giving birth
- Undergoing gynaecological or prostate surgery
- Pelvic floor inactivity (i.e. not using your muscles enough)
- Pelvic floor overactivity (i.e. using your muscles excessively often with a subsequent inability to relax your pelvic floor muscles)
Pelvic floor dysfunction is very common, typically affecting females more commonly than males with approximately 50% of women affected at some stage in their lives. In Australia, approximately 4.8 million people (both males and females) of all ages and backgrounds are affected by pelvic floor dysfunction with subsequent incontinence.
Cause of pelvic floor dysfunction
Pelvic floor dysfunction typically occurs when the pelvic floor muscles are weakened, stretched excessively or too tight (i.e overactive). The following factors may work in isolation or combination to cause pelvic floor dysfunction:
- Being pregnant and giving birth (with increased risk with multiple births and women undergoing caesarean delivery also being affected)
- Pelvic floor inactivity (i.e. not using your pelvic floor enough)
- Excessive use of the Pelvic floor (i.e. using the pelvic floor too much, with a subsequent inability to relax)
- Being overweight
- Heavy lifting or high impact activity
- Undergoing gynaecological or prostate surgery
- A history of lower back pain
- Long term constipation and straining to empty the bowels
- A chronic cough or sneeze (e.g. in smokers, asthmatics or those suffering hay fever or bronchitis)
- A past history of injury to the pelvic region such as a pelvic fracture (e.g. due to a fall) or pelvic radiotherapy (which may damage pelvic floor tissue or associated nerves)
- Poor posture
- Menopause
- A sedentary lifestyle
- Genetic predisposition (i.e. inherited deficiency in collagen – the protein responsible for giving connective tissue strength)
- Age (more common with increasing age)
Signs and symptoms of pelvic floor dysfunction
The signs and symptoms of pelvic floor dysfunction can vary significantly between individuals based on the type and severity of the dysfunction. Symptoms of a weak or excessively stretched pelvic floor may include:
- Urinary incontinence (such as leaking urine when you cough, sneeze, laugh, shout, run, jump, walk, exercise, push, pull, lift something heavy, change positions or during everyday activities such as gardening or sport)
- Not being able to hold on when you need to go to the toilet
- Feeling like you need to go to the toilet very frequently or in a hurry
- Accidentally losing control of your bladder or bowel
- Unintentionally passing wind
- Pelvic pain or pain during intercourse
- Prolapse or sagging of internal organs. In women, this may be felt as a heaviness, dragging, discomfort or bulge in the vagina. In men, this may be felt as a bulge in the rectum or a feeling of needing to empty their bowels but not actually needing to go).
Symptoms of an overactive pelvic floor may include:
- Difficulty emptying your bowel or bladder
- Straining when moving your bowels
- Pelvic pain or pain during intercourse
Diagnosis of pelvic floor dysfunction
A thorough subjective and objective examination from a physiotherapist with postgraduate training in women’s and men’s health is usually sufficient to diagnose pelvic floor dysfunction. This will often entail real time ultrasound investigation and sometimes digital assessment. In some cases, referral to a specialist may be required for further evaluation and testing. This may include EMG or nerve conduction studies, X-ray or MRI investigation, manometry (a test involving the insertion of a small catheter with a balloon on one end into the rectum), balloon expulsion tests or a variety of other examination procedures.
Treatment of pelvic floor dysfunction
Underactive or weak pelvic floor

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Overactive pelvic floor

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Physiotherapy for pelvic floor dysfunction

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Other intervention for pelvic floor dysfunction
Despite appropriate physiotherapy management, some patients with pelvic floor dysfunction do not improve adequately or, in some cases, continue to deteriorate. When this occurs, other intervention may be required. This may include:
- Further investigations such as an ultrasound, X-ray, MRI, digital assessment, EMG or nerve conduction studies, manometry, balloon expulsion testing or a variety of other investigation procedures.
- Assessment from a specialist
- Pharmaceutical intervention
- The use of pads, catheters , condom drainage (for men) or mattress protectors for incontinence containment and management
- The use of support pessaries
- Surgical intervention (in rare cases, with severe symptoms that are unresponsive to conservative measures)
Exercises for pelvic floor dysfunction
The following pelvic floor exercises are frequently prescribed in physiotherapy clinical practice to improve strength and control of the pelvic floor muscles and to prevent or treat pelvic floor dysfunction. You should discuss the suitability of these pelvic floor exercises with your physiotherapist prior to beginning them. Generally they should be performed 3 times daily provided they do not cause or increase symptoms.
Pelvic Floor Exercises – Neutral Spine
Begin your pelvic floor exercises by setting yourself up in a comfortable position that allows relaxation of your global muscles, isolated pelvic floor activation and maintenance of your spine in a neutral position.
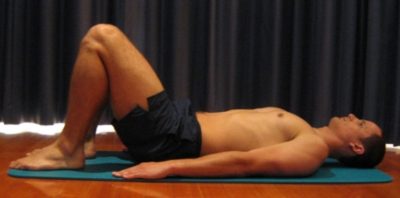
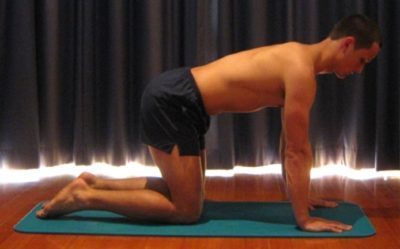
For those who are new to pelvic floor exercises, it is generally most appropriate to begin either lying on your back or whilst sitting, in neutral spine. Other alternative starting positions may include four-point kneeling or lying on your side.
Once you are confident with activating your pelvic floor in these positions, you can progress to other more functional positions such as standing or whilst walking etc.
Achieving neutral spine
Neutral Spine refers to the position whereby your spine is in optimal postural alignment (figures 1 – 4). Generally, neutral spine can be obtained by ensuring the following:
- Think about maintaining a tall, long spine with minimal effort
- There should be a straight line from your ears, to your shoulders, to your hips
- Your chin should be tucked in slightly with your eyes and nose facing forwards.
- Your shoulder blades should be back slightly
- Your upper back relatively straight
- There should be a slight curve in your lower back


How to contract your pelvic floor muscles
Once you have positioned yourself in neutral spine and in an ideal starting position for you (i.e. generally lying on your back or sitting), identify the 2 or 3 parts of your pelvic floor as follows:
- The muscles that control the flow of urine – to identify how to contract these muscles for training, try to stop the flow of urine mid-stream next time you are urinating. Hold these muscles for a few seconds and then relax. This should not be used as an exercise and should only be used for muscle identification.
- The muscles that control your anal sphincter – these muscles can be activated by tightening the muscles around your anus as though you are trying to stop the passing of wind. Squeeze and lift these muscles inwards and upwards. Hold these muscles for a few seconds and then relax.
- For women – the muscles that surround your vagina – the easiest way to tighten these muscles correctly is by inserting your fingers into the vagina and then try to squeeze them. Slowly pull your fingers out and use your pelvic floor muscles to resist. If this is not comfortable for you, try to tighten these muscles by squeezing and lifting the muscles in and around this opening. Hold for a few seconds and then relax.
When performing pelvic floor exercises, it is generally most beneficial to activate all parts of your pelvic floor simultaneously. This can be achieved by gently tightening the muscles around your back passage and at the same time squeezing and lifting the muscles around your bladder outlet (and vagina – in women) as though you are trying to stop the flow of urine.
Poor recruitment patterns – what to avoid
When learning how to contract your pelvic floor muscles, it is common for patients to perform trick movements or poor recruitment patterns (contracting muscles other than the pelvic floor). Some common errors / poor recruitment patterns that should be avoided include:
- Lifting or shrugging your shoulders
- Tightening other openings such as the eyes / mouth
- Global muscle contraction such as tightening the buttocks, thighs or abdominals (e.g. pulling your belly button in).
- Bearing down – i.e. some people mistakenly push down on their pelvic floor when performing pelvic floor exercises, which can exacerbate pelvic floor problems.
- Holding your breath
Initial Pelvic Floor Exercise
You should discuss the suitability of this initial pelvic floor exercise with your physiotherapist prior to commencing. Generally it should be performed 3 times daily provided it does not cause or increase symptoms.
Beginner pelvic floor activation
Begin lying or sitting in neutral spine (figures 1 or 2) with minimal muscular effort. Relax your global muscles and ensure you are breathing normally. Tighten the muscles around your back passage as if you are trying to stop the passing of wind. Slowly and gently squeeze and lift the muscles upwards and inwards and then relax (ensuring you feel a definite letting go). Repeat 5 – 10 times, 3 times daily.
Intermediate Pelvic Floor Exercise

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
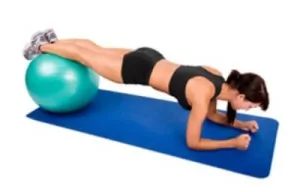
Advanced Pelvic Floor Exercise

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Functional Progressions

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Rehabilitation Protocol for pelvic floor dysfunction

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
 Physiotherapy products for pelvic floor exercises
Physiotherapy products for pelvic floor exercises
To purchase physiotherapy products to assist with pelvic floor dysfunction click on the relevant link or visit the PhysioAdvisor Shop.
 More Exercises
More Exercises
- Pelvic Floor Exercises
- What is Clinical Pilates?
- Pilates – Before You Start
- Beginner Pilates Exercises
- Intermediate Pilates Exercises
- Advanced Pilates Exercises
- Pilates Foam Roller Exercises
 Find a Physio to assist with pelvic floor dysfunction
Find a Physio to assist with pelvic floor dysfunction
Find a physiotherapist in your local area who can assist with pelvic floor dysfunction treatment. Your physiotherapist can also assist with pelvic floor exercises and ensure you are activating your muscles correctly. Ideally you should see a physiotherapist specialising in continence and pelvic floor retraining.
Become a PhysioAdvisor Member

Link to this Page
If you would like to link to this article on your website, simply copy the code below and add it to your page:
<a href="https://physioadvisor.com.au/injuries/hip-groin/pelvic-floor-dysfunction-incontinence”>Pelvic Floor Dysfunction – PhysioAdvisor.com</a><br/>View detailed physiotherapy information on pelvic floor dysfunction and incontinence including symptoms, diagnosis, treatment and pelvic floor exercises.
Return to the top of Pelvic Floor Dysfunction.









