Gluteal Tendinopathy
Updated:
What is gluteal tendinopathy?
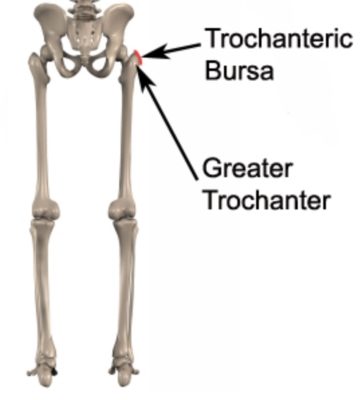
Gluteal tendinopathy is a common condition seen in clinical practice. It is characterized by microscopic damage, degeneration and often pain and swelling in one or more of the gluteal tendons at their attachment point to the outer hip (greater trochanter – figure 1).
Anatomy of gluteal tendinopathy
The thigh bone (femur) has a bony process located at the outer aspect of the top of the bone known as the greater trochanter (figure 1). The greater trochanter is the outer most point of the hip and provides the attachment point for several gluteal muscles. Two of the gluteal muscles (gluteus medius and minimus) originate from the pelvis and insert into the greater trochanter via their respective gluteal tendons (figure 2). Located between the largest gluteal muscle (gluteus maximus) and greater trochanter is a bursa known as the trochanteric bursa (figure 1). A bursa is a thin sac filled with lubricating fluid and is designed to reduce friction between adjacent soft tissue layers.
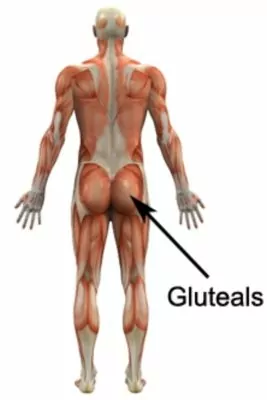
The gluteal muscles are primarily responsible for moving the hip and stabilizing the pelvis during activity and are particularly active during walking and running (especially on uneven surfaces or up or down hills / stairs), jumping, lunging, squatting, twisting and standing. They’re also under significant stress when lying upon them or when crossing the legs. When the gluteal muscles contract or are under stress, stretching or compressive forces are placed on the gluteal tendons. Pressure may also be placed on the gluteal tendons due to a direct blow. When these forces are excessive due to too much repetition, prolonged or high force, irritation and gradual degeneration / microscopic damage / swelling of the gluteal tendons may occur. This condition is known as gluteal tendinopathy.
The forces involved in Gluteal tendinopathy also place stress on the trochanteric bursa (which lies right next to the gluteal tendons). As a result, trochanteric bursitis frequently co-exists with gluteal tendinopathy.
Causes of gluteal tendinopathy
Gluteal tendinopathy typically occurs due to overuse. This may be due to repetitive, prolonged or forceful activities placing stress on the gluteal tendons such as: excessive walking or running (especially up or down hills or stairs, on uneven surfaces or with change of direction), twisting, jumping, hopping, squatting, lunging activities, excessive periods standing or sitting (especially in low chairs or with legs crossed), lifting or carrying or due to prolonged pressure on the tendons (such as excessive side-lying particularly on hard surfaces). Occasionally, the condition may occur suddenly due a direct blow to the point of the hip (such as a fall onto a hard surface).
Signs and symptoms of gluteal tendinopathy
Gluteal tendinopathy usually causes pain or discomfort in the outer aspect of the hip and buttock. Sometimes, pain may radiate down the outer thigh as far as the knee. In less severe cases, patients may only experience an ache or stiffness in the hip that increases with rest following provocative activities placing stress on the gluteal tendons. These activities may include standing or walking excessively (especially up or down hills / stairs, on uneven surfaces or with change of direction) side lying excessively (especially on hard surfaces), running, jumping, squatting, lunging, twisting (i.e. change of direction activities), prolonged sitting (especially cross legged or in low chairs), lifting or carrying, getting in and out of the car. The pain associated with this condition may also warm up with activity in the initial stages of injury.
In more severe cases, patients may experience symptoms that increase during sport or activity, adversely affecting performance. Patients with gluteal tendinopathy typically experience pain on firmly touching the gluteal tendons (usually at their attachment point to the greater trochanter) and often trochanteric bursa (figure 1). Occasionally, a feeling of lower limb weakness may also be present particularly when attempting to climb stairs, perform a lunge or squat or accelerate whilst running.
Diagnosis of gluteal tendinopathy
A thorough subjective and objective examination from a physiotherapist may be sufficient to diagnose gluteal tendinopathy. Further investigations such as an Ultrasound, X-ray, CT or MRI scan are often required to assist with diagnosis and assess the severity of the condition. Combined ultrasound and X-ray are usually the investigation of choice.
Treatment for gluteal tendinopathy

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Prognosis of gluteal tendinopathy
Most patients with this condition make marked progress and heal well with appropriate physiotherapy and return to normal function in a number of weeks. Occasionally, rehabilitation can take significantly longer and may take many months in those who do not follow appropriate rehabilitation instructions correctly. Early physiotherapy treatment is vital to hasten recovery in all patients with gluteal tendinopathy.
Contributing factors to the development of gluteal tendinopathy
There are several factors which can predispose patients to developing this condition. These need to be assessed and corrected with direction from a physiotherapist. Some of these factors include:
- overuse – repetitive / prolonged or excessive stress on the gluteal tendons (e.g. walking, running, cycling, weightlifting, sidelying on the affected side etc.)
- joint stiffness (particularly the hip)
- lack of strength or flexibility in the hip muscles (particularly the gluteals)
- increasing age (tendons become less flexible and more prone to injury as we age).
- poor posture, biomechanics or movement patterns (e.g. during standing, walking or running)
- inappropriate or excessive training
- inadequate warm up
- previous lower limb injury (such as the buttock or hip, especially with inadequate rehabilitation)
- medical conditions such as osteoarthritis
- poor pelvic or core stability
- neural tightness
- leg length discrepancy
Physiotherapy for gluteal tendinopathy
Physiotherapy rehabilitation and treatment is essential to accelerate healing, minimise the probability of recurrence and ensure an optimal outcome. Treatment may entail:
- education
- activity modification / pacing advice
- the use of crutches
- manual therapy
- dry needling
- taping
- electrotherapy (e.g. ultrasound, TENS etc)
- joint mobilization
- the use of ice or heat
- exercises to improve strength, function, core stability and flexibility
- biomechanical correction where indicated (e.g. the use of orthotics)
- anti-inflammatory advice
- a gradual return to activity program
Other intervention for gluteal tendinopathy
Despite appropriate physiotherapy management, a small percentage of patients with gluteal tendinopathy may not improve adequately. When this occurs your physiotherapist or G.P will advise on the best course of management. This may entail investigations such as X-rays, ultrasound, MRI or CT scan, medication prescription, corticosteroid injection or referral to appropriate medical authorities (e.g. sports physician, orthopaedic specialist etc.) who can advise on any other interventions that may be required to improve the condition.
Exercises for gluteal tendinopathy
Patients with gluteal tendinopathy are often prescribed the following exercises. However, it’s important to discuss the suitability of these exercises with your physiotherapist before commencement. These exercises should generally be performed 2 – 3 times per day, and only if they do not cause or increase symptoms. Your physiotherapist will guide you on when it’s appropriate to start with the initial exercises and progress to intermediate and advanced exercises. As a general rule, adding more exercises or progressing to advanced ones should only happen if there’s no increase in symptoms.
Initial Exercises
Hip Extension in Standing
Begin this exercise standing at a bench or chair for balance as demonstrated (figure 3). Keeping your back and knee straight, slowly take your leg backwards gently, tightening your bottom muscles (gluteals). Begin with 5 repetitions and gradually build to 15 over a number of days provided the exercise is pain free. Begin by only performing the exercise standing on the uninjured leg and taking the injured leg backwards. Eventually perform the exercise on both sides provided there is no increase in discomfort.

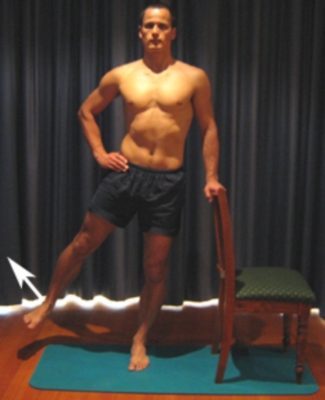
Hip Abduction in Standing
Begin this exercise standing at a bench or chair for balance as demonstrated (figure 4). Keeping your back and knee straight, slowly take your leg to the side gently. Perform 5 – 15 repetitions provided the exercise is pain free. Begin by only performing the exercise standing on the uninjured leg and taking the injured leg to the side. Eventually perform the exercise on both sides provided there is no increase in discomfort.
Intermediate Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Advanced Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Other Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Rehabilitation Protocol for gluteal tendinopathy

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Physiotherapy products for gluteal tendinopathy
Some of the most commonly recommended products by physiotherapists to hasten healing and speed recovery in patients with this condition include:
To purchase physiotherapy products for gluteal tendinopathy click on one of the above links or visit the PhysioAdvisor Shop.
Find a Physio
Find a physiotherapist in your local area who can treat this condition.
More Information
- View Gluteal Strengthening Exercises.
- View more Gluteal Stretches.
- View Core Stability Exercises.
- View detailed information about How to use Crutches.
- View detailed information about the R.I.C.E. Regime.
- View detailed information about when to use Ice or Heat.
- View a Return to Running Program that is often used in rehabilitation.
Become a PhysioAdvisor Member
-
 Individual Membership (12 Months)$59.95 for 1 year
Individual Membership (12 Months)$59.95 for 1 year -
 Individual Membership (3 Months)$39.95 for 3 months
Individual Membership (3 Months)$39.95 for 3 months -
 Individual Membership (Yearly)$49.95 / year
Individual Membership (Yearly)$49.95 / year -
 Individual Membership (Monthly)$15.95 / month
Individual Membership (Monthly)$15.95 / month

Link to this Page
If you would like to link to this article on your website, simply copy the code below and add it to your page:
<a href="https://physioadvisor.com.au/injuries/hip-groin/gluteal-tendinopathy”>Gluteal Tendinopathy – PhysioAdvisor.com</a><br/>
Return to the top of Gluteal Tendinopathy.






