Iliotibial Band Syndrome
Updated:
(Also known as ITB Syndrome, Iliotibial Band Friction Syndrome, Iliotibial Syndrome, ITBFS, Runner’s Knee)
What is Iliotibial band syndrome?
Iliotibial band syndrome is a condition that commonly presents in runners and typically causes pain at the outer (lateral) aspect of the knee where the iliotibial band (ITB) crosses the knee joint. Iliotibial band syndrome describes a condition whereby the iliotibial band rubs against a bony prominence at the outer aspect of the knee (the femoral epicondyle – figure 1) and typically causes inflammation and damage to the ITB and local tissue.
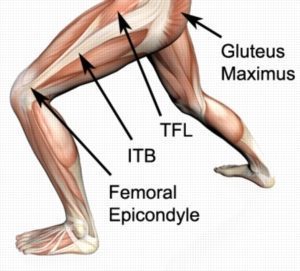
The iliotibial band is a long band of connective tissue than runs down the outer aspect of the thigh (figure 1). It originates from two muscles on the outer aspect of the hip (the tensor fascia latae (TFL) and gluteus maximus – figure 1) and runs down past the knee to attach into the lower leg bone (tibia). As the ITB crosses the knee, it overlies a bony prominence known as the femoral epicondyle (figure 1). As the knee bends and straightens the ITB flicks over this bony prominence which places friction on the ITB and local soft tissue. If this friction becomes excessive or too repetitive (such as during excessive running) the ITB or local tissue can become damaged or inflamed resulting in pain. When this occurs the condition is known as Iliotibial band syndrome.
Signs and symptoms of Iliotibial band syndrome
Patients with iliotibial band syndrome usually experience pain at the outer aspect of the knee. Patients usually experience an ache that may increase to a sharper pain with activity. Pain is typically experienced during activities that bend or straighten the knee particularly whilst weight bearing. Pain may be worse first thing in the morning or following activity (once the body has cooled down). This may be associated with knee stiffness and can sometimes cause the patient to limp.
Activities that frequently aggravate symptoms include running (particularly longer runs, downhill running or running on cambered surfaces), walking (particularly up and down stairs or hills), squatting or jumping. Patients with iliotibial band syndrome typically experience pain when firmly touching the outer aspect of the knee (femoral epicondyle – figure 1). In more severe cases, swelling may be present at the outer aspect of the knee along with an associated grinding sound when bending or straightening the knee. Occasionally, patients may also experience episodes of the knee giving way or collapsing due to pain.
Causes of Iliotibial band syndrome
Iliotibial band syndrome is an overuse injury usually caused by excessive running. It typically occurs due to excessive training volumes, intensities, durations or frequencies or following a sudden increase in training or change in surface or footwear. Any overuse activity which involves repetitive knee bending and straightening, particularly in weight bearing, can contribute to the development of the condition (i.e. walking, running, cycling, rowing). Iliotibial band syndrome is commonly seen in marathon runners, athletes, triathletes and footballers.
Diagnosis of Iliotibial band syndrome
A thorough subjective and objective examination from a physiotherapist is usually sufficient to diagnose Iliotibial band syndrome. Investigations such as an ultrasound or MRI may be used to assist with diagnosis and to rule out other pathologies.
Treatment for Iliotibial band syndrome

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Contributing factors to the development of Iliotibial band syndrome
There are several factors which can predispose patients to developing Iliotibial band syndrome. These need to be assessed and corrected with direction from a physiotherapist. Some of these factors include:
- excessively tight ITB
- muscle tightness (particularly TFL, gluteus maximus, vastus lateralis or calf)
- excessive or inappropriate training or activity
- inadequate recovery periods from sport or activity
- inadequate warm up
- inadequate rehabilitation following a previous lower limb injury
- a sudden change in training volume, intensity, frequency, duration, conditions or surfaces
- abnormal running biomechanics
- excessive pronation (i.e. flat feet)
- poor pelvic or core stability
- muscle weakness (especially the VMO and gluteal muscles)
- muscle strength imbalances
- tightness in specific joints (hip, knee or ankle)
- inappropriate footwear or surfaces
- poor running technique

Physiotherapy for Iliotibial band syndrome
Physiotherapy treatment for Iliotibial band syndrome is vital to hasten the healing process, ensure an optimal outcome and reduce the likelihood of recurrence. Treatment may comprise:
- soft tissue massage (particularly to the ITB – figure 4)
- joint mobilization (involving the knee, patellofemoral joint, superior tibiofibular joint, ankle or hip)
- dry needling
- electrotherapy (e.g. ultrasound)
- ice or heat treatment
- progressive exercises to improve flexibility, strength and balance
- activity modification advice
- the use of crutches
- the use of an appropriate ITB Strap
- biomechanical correction
- anti-inflammatory advice
- clinical Pilates and core stability exercises
- footwear advice
- bike setup advice (for cyclists)

Prognosis of Iliotibial band syndrome
Most patients with this condition heal well with appropriate physiotherapy. Resolution of symptoms can usually be achieved provided the contributing factors have been identified and appropriate action taken to address them. However, recovery can be a lengthy process and may take several months in those patients who have had their condition for a long period of time. Minor cases of this condition that are identified and treated early can usually settle within a few weeks. Early physiotherapy treatment is therefore vital to hasten recovery and ensure an optimal outcome.
Other intervention for Iliotibial band syndrome
Despite appropriate physiotherapy management, some patients with Iliotibial band syndrome do not improve. When this occurs the treating physiotherapist or doctor can advise on the best course of management. This may include further investigations, such as an ultrasound or MRI scan, pharmaceutical intervention, a corticosteroid injection, or a referral to an orthopaedic specialist who will advise on any procedures that may be appropriate to improve the condition. Surgery to release the ITB may sometimes be considered in severe cases, where patients have failed to improve through conservative means. A review with a podiatrist may also be indicated for the prescription of orthotics to correct any foot posture abnormalities.
Exercises for Iliotibial band syndrome
The following exercises are commonly prescribed to patients with iliotibial band syndrome. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 3 times daily once the physiotherapist has indicated it is safe to do so and only provided they do not cause or increase symptoms.
Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate and advanced exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms.
Initial Exercises
ITB Stretch
Cross your injured leg behind your uninjured leg, taking it as far as you comfortably can (figure 5). Then push your hips to the side of your leg to be stretched as far as you can go without pain and provided you feel no more than a mild to moderate stretch in your outer thigh / hip (ITB). Keep your back straight. Hold for 15 seconds and repeat 4 times at a mild to moderate stretch (or as far as you can go without any pain).

Static (VMO) Quadriceps Contraction
With your knee relatively straight, slowly tighten the muscle at the front of your thigh (quadriceps) by pushing your knee down into a small rolled up towel (figure 6). Put your fingers on your inner (medial) quadriceps (VMO) to feel the muscle tighten during the contraction. Hold for 5 seconds and repeat 10 times as firmly as possible without increasing your symptoms.

Calf Stretch
With your hands against the wall, place your leg to be stretched behind you as demonstrated (figure 7). Keep your heel down, knee straight and feet pointing forwards. Gently lunge forwards as far as you can go without pain and provided you feel no more than a mild to moderate stretch in the back of your calf / knee. Hold for 15 seconds and repeat 4 times at a mild to moderate stretch provided the exercise is pain free.


Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Intermediate Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Advanced Exercises

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now
Rehabilitation Protocol for Iliotibial band syndrome

Members Only ContentBecome a PhysioAdvisor Member to gain full access to this exclusive content. For more details see Become a Member. Already a member? Login Now

Physiotherapy products for Iliotibial band syndrome
Some of the most commonly recommended products by physiotherapist for patients with Iliotibial band syndrome include:
To purchase physiotherapy products for Iliotibial band friction syndrome click on one of the above links or visit the PhysioAdvisor Shop.
 More Exercises
More Exercises
- ITB Flexibility Exercises
- Quadriceps Flexibility Exercises
- Lower Body Foam Roller Exercises
- Gluteal Strengthening Exercises
- Quadriceps Strengthening Exercises
- Pilates Exercises(to improve core stability)
- Core Stability Exercises
- Leg Strengthening Exercises
- Leg Stretches
- Balance Exercises
- Cardiovascular Exercise
- Lower Body Massage Ball Exercises
 Recommended Reading
Recommended Reading
- How to use Crutches
- Ice or Heat
- The R.I.C.E. Regime
- Choosing a Running Shoe
- Do I Need Orthotics?
- Return to Running
- Returning to Sport
- Knee Diagnosis Guide
 Find a Physio
Find a Physio
Find a Physiotherapist in your local area who can treat Iliotibial band syndrome.
Become a PhysioAdvisor Member

Link to this Page
If you would like to link to this article on your website, simply copy the code below and add it to your page:
<a href="https://physioadvisor.com.au/injuries/knee/iliotibial-band-syndrome”>Iliotibial Band Syndrome – PhysioAdvisor.com</a><br/>Iliotibial band syndrome is a condition that causes pain at the outer aspect of the knee. Learn more about its causes, treatment & exercises at PhysioAdvisor.
Return to the top of Iliotibial Band Syndrome.